Why are Black patients less likely than white patients to be prescribed opioids for acute pain in the emergency department (ED)? While many theories have been put forward (ranging from racial differences in patients’ pain management preferences to providers’ false beliefs in biological differences between racial groups), the specific mechanisms underpinning these disparities are unclear.
We used data collected for Life STORRIED, a multicenter randomized controlled trial (RCT) to clarify the role of patient pain management preference and to test the effectiveness of an intervention in reducing these disparities. We studied 1,302 patients presenting to the EDs of four academic medical centers with acute musculoskeletal back pain or renal colic. Even in the controlled setting of an RCT, we found that Black patients presenting to the ED were less than half as likely as similar white patients to be prescribed opioids for acute pain.
Patient preferences did not seem to explain this disparity. We found nearly identical disparities among patients who preferred opioids and among those who did not prefer opioids. Even among patients who preferred to not receive opioids, white patients were more likely than Black patients to be prescribed opioids.
Next, we tested the effectiveness of an intervention in reducing this disparity. Previous research, primarily in the area of employment discrimination, has proposed a theory called statistical discrimination. According to this theory, disparities emerge when decision makers apply generalizations about a group to individual members of that group to fill in a knowledge gap. Inaccurate statistical discrimination occurs when generalizations are based on false beliefs about a group. We hypothesized that this theory of discrimination may have particular relevance in the ED where providers are often missing important data about the patients who they are treating.
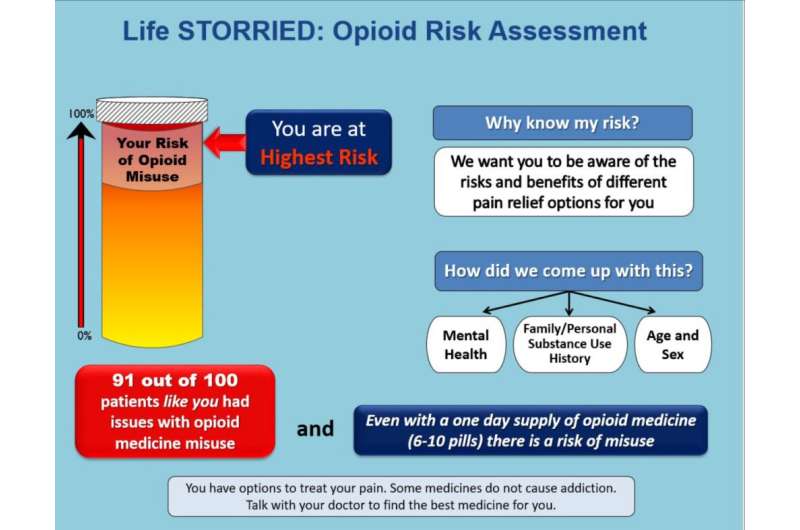
To test whether statistical discrimination may play a role in generating opioid prescribing disparities, we analyzed the impact of a clinician-facing intervention that consisted of a display containing information about each enrolled patient’s analgesia treatment preference, as well as the risk of future opioid misuse (see figure 1 for a sample display). We found that, even when providers were shown information about their patients’ treatment preferences and risk of misusing opioids, Black patients remained less likely to be prescribed opioids.
When we analyzed our data based on opioid preference and enrollment in our treatment arm, an unexpected pattern emerged; among those who did not prefer opioids, White patients were more likely than Black patients to receive a prescription for opioids in the treatment arm (in which clinicians were given additional information about their patients’ preferences and opioid-related risks) but not in the control arm.
Our findings suggest that statistical discrimination is not generating these disparities. In fact, we found that providing prescribers with additional information about their patients was associated with increased disparities among patients who did not prefer opioids. Most patients in our sample had very low opioid risk scores, so one potential explanation is that providers applied this additional, largely reassuring data in a biased and differential way in their interactions with Black and white patients.
Safe opioid prescribing is important, especially given the ongoing opioid overdose crisis. It is also important, however, that opioid stewardship efforts do not worsen access to effective pain control for Black patients. With the goal of achieving both equitable and safe access to opioids, further work is needed to design and test interventions to mitigate structural racism and disparities in acute pain management.
Source: Read Full Article



