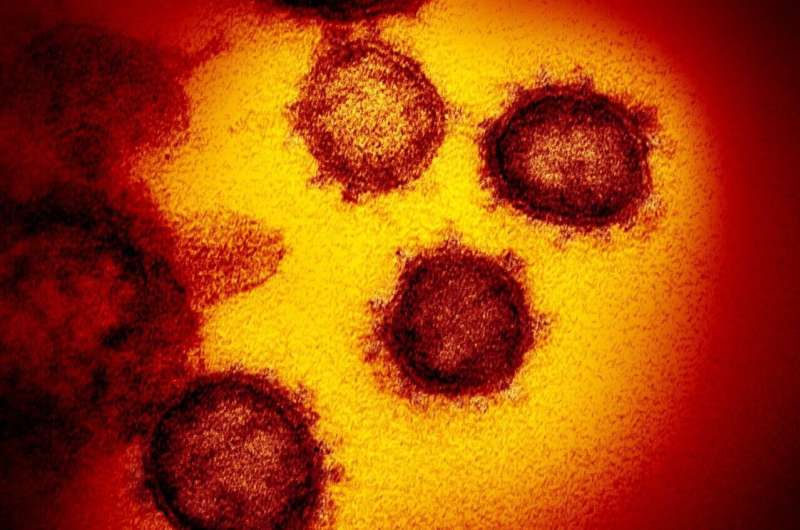
People in the U.S. who live in socially vulnerable neighborhoods, which includes communities with higher rates of poverty, crowded living situations and/or a higher proportion of people from diverse racial and ethnic groups, had higher rates of death and cardiac events such as a heart attack or stroke when hospitalized with COVID-19, according to preliminary research presented today at the American Heart Association’s Scientific Sessions 2021.
“Based on what we have seen with COVID-19 infections, we expected worse outcomes among hospitalized patients from more vulnerable neighborhoods,” said Shabatun Islam, M.D., lead author of the study and a cardiology fellow at Emory University School of Medicine in Atlanta. “However, we thought the findings would be partially explained by the patients’ preexisting health conditions or how sick they were when they were admitted to the hospital, yet this was not the case.”
Throughout the pandemic, evidence has shown that people from diverse racial and ethnic groups have had worse outcomes from COVID -19 infection. Population-based studies have also found that people from socially vulnerable neighborhoods had worse outcomes from COVID -19. However, there has been limited research focused specifically on whether hospitalized COVID-19 patients from socially vulnerable neighborhoods had more complications or worse outcomes while hospitalized.
The U.S. Centers for Disease Control and Prevention’s Social Vulnerability Index (SVI) scale ranks communities based on 15 factors, including:
- socioeconomic status, which includes households below the national poverty level (as determined annually by the U.S. Department of Health and Human Services with adjustments based on the number of household members), high levels of unemployment and low education level (lacking a high school diploma);
- household composition and disability, which includes households with single-parents, if anyone in the household serves in the military, individuals with disabilities, elderly adults and children;
- race/ethnic group and language within the household, including if English is not the first or primary language in the household; and
- housing type and transportation, which includes multi-unit structures, mobile homes, crowded conditions or group quarters and whether most households have a personal vehicle or primarily use public transportation.
The SVI, calculated every two years, was created in 2011 mainly to guide public health officials and other planners in identifying at-risk communities and communities that may need extra support before, during and after natural disasters and public health crises.
The researchers in this study used information from the American Heart Association’s COVID-19 Cardiovascular Disease Registry, which captures data about adult patients hospitalized with COVID-19 infection—including those with and without a history of cardiovascular disease. Records on patients’ clinical characteristics, medications, treatments, labs, vitals, biomarkers and outcomes are included in the registry.
Health data for almost 20,000 people hospitalized with COVID-19 between January and November 2020 across 107 U.S. hospitals were extracted from the Association’s COVID-19 CVD Registry and analyzed for this study to determine if SVI impacted patients’ cardiac outcomes. Researchers discovered that the patients hospitalized with COVID-19 who resided in the most socially vulnerable neighborhoods had higher rates of in-hospital death and cardiovascular events such as heart attack, stroke or new-onset heart failure.
About 40% of the patients in the analysis lived in areas ranked within the highest national quartile of Social Vulnerability Index, meaning there were even lower levels of poverty, higher proportion of residents from diverse racial and ethnic groups, and higher degrees of inadequate housing and transportation compared to other socially vulnerable communities. When these patients were compared to patients who lived in the areas ranked within the lowest quartile of Social Vulnerability Index, they were found to be slightly younger, and there was a higher percentage of Black adults. Additionally, they were more likely to be women and less likely to have private health insurance. However, after accounting for factors such as age, sex, race/ethnicity, insurance status and other medical conditions, the analysis found that living in areas with the highest SVI appeared to be independently associated with an increased likelihood of having a cardiac event or dying while hospitalized with COVID-19.
“It is widely known that an individual’s neighborhood of residence impacts their health,” said Islam. “As physicians, it’s important for us to recognize that people living in vulnerable neighborhoods often experience high rates of adverse health outcomes even when everything else may be the same. Additionally, it is important to strive to provide each patient with the resources and support to improve overall health and health outcomes. It is not always clear what specifically may be the most helpful to help support our patients, so this is definitely an area where future research is needed.”
“Unfortunately, I’m not surprised by the findings of this research. Getting into the why, how, and which social factors are most consequential in affecting health and then putting our patients in contact with the resources to help them are key for health care professionals,” said Michelle A. Albert, M.D., M.P.H., FAHA, president-elect of the American Heart Association, and professor of medicine, associate dean of admissions and director of the CeNter for the StUdy of AdveRsiTy and CardiovascUlaR DiseasE (NURTURE Center) at the University of California, San Francisco. “Addressing health disparities is going to take a multi-pronged approach of societal solutions, such as building community relationships, increasing diversity in the health care workforce, and strengthening research funding and clinical care focused on social factors and their impact on health. These solutions will require sustained efforts over time; there’s a lot of work to be done.”
While this study was not focused on the root cause of health disparities and social determinants of health, the American Heart Association’s 2020 Presidential Advisory, “Call to Action: Structural Racism as a Fundamental Driver of Health Disparities,” specifically identifies structural racism as a cause, both in the past and presently, for persistent health disparities in the U.S. Structural racism is defined as the normalization and legitimization of an array of dynamics—historical, cultural, institutional and interpersonal—that routinely advantage white people while producing cumulative and chronic adverse outcomes for people of color.
Source: Read Full Article