The elderly are five times more likely than younger adults to develop problems related to constipation.
Causes of constipation in the elderly
Some of the reasons for this propensity include poor diet, lack of adequate fluids in diet, lack of exercise, the use of certain drugs to treat other medical conditions, and poor bowel habits.
In addition there is a psychological angle and many older adults are excessively concerned about their bowel movements and constipation is frequently an imaginary ailment.
There is often a lack of interest in eating that is seen in single or widowed older people. This leads to over use of convenience foods, which tend to be low in fiber.
Loss of teeth may further make eating regular meals difficult. Many older adults thus choose soft, processed foods that are low in fiber.
Many older adults suffer from urinary incontinence and stress incontinence. They may take inadequate fluids in order to avoid urinating. The fluids are also deficient in diet if the elderly are not eating regular or balanced meals. Water and other fluids add bulk to stools relieving constipation and making stools soft.
Another major cause for constipation in the elderly is prolonged bed rest or being bed ridden for example, after an accident or during an illness. Lack of movement and exercise may contribute to constipation.
Drugs prescribed for several medical conditions may lead to constipation among the elderly. Some of these include antidepressants, antacids containing aluminum or calcium, antihistamines, diuretics, and anti-Parkinsonism drugs.
Fearing constipation is common among the elderly and this sometimes leads older people to depend heavily on stimulant laxatives. These are habit forming and the bowel movements begin to depend on laxatives and over time, the natural mechanisms fail to work without the help of drugs. Habitual use of enemas also can lead to a loss of normal bowel movements.
Types of constipation among elderly
Normal transit constipation
This is the most common subtype of primary constipation. Here, despite the stool passing through the colon at a normal rate, patients perceive difficulty in evacuating their bowels. This is commonly seen along with irritable bowel syndrome with constipation. The primary distinction between chronic constipation and Irritable bowel syndrome (IBS) is the abdominal pain or discomfort seen in IBS.
Slow-transit constipation
This condition is seen more commonly among women. There are infrequent bowel movements, limited urgency, or straining to defecate. The colonic movements are slow.
Pelvic floor dysfunction
There is a problem in the muscles of the pelvic floor or around the anus (anal sphincter). These patients have a poor ability to co-ordinate these muscles during defecation. There is a feeling of incomplete evacuation. There is an overlap of this condition with slow transit colon.
Diagnosis of constipation in elderly
Diagnosis begins with detailed history and physical examination. Drug induced constipation, constipation due to prolonged inactivity and changes in diet and fluid intake may be diagnosed from history.
New onset constipation, worsening of constipation, blood in the stools, unexplained weight loss, fever, nausea, vomiting, loss of appetite, family history of inflammatory bowel disease or colon cancer in older adults over the age of 50 years need to be evaluated carefully for other conditions underlying constipation including colon and rectal cancers.
A general examination is next undertaken to evaluate the presence of other causes of constipation. Other causes that may affect other body systems and manifest as constipation include:
- heart diseases like heart failure
- Diabetes mellitus
- hypothyroidism (underactive thyroid)
- hypercalcaemia (increased blood calcium)
- hypokalaemia (low blood potassium)
- hypermagnesaemia (increased blood magnesium)
- hyperparathyroidism (overactive parathyroid glands) etc.
Some muscle and nerve disorders that may cause constipation include dermatomyositis, systemic sclerosis, autonomic neuropathy, Parkinson’s disease, spinal cord lesion (tumours or injury) and presence of dementia and depression.
Some diseases of the gastrointestinal system may also lead to constipation. These include anal fissure, diverticular disease, strictures, irritable bowel disease, rectal prolapsed, volvulus, megacolon etc.
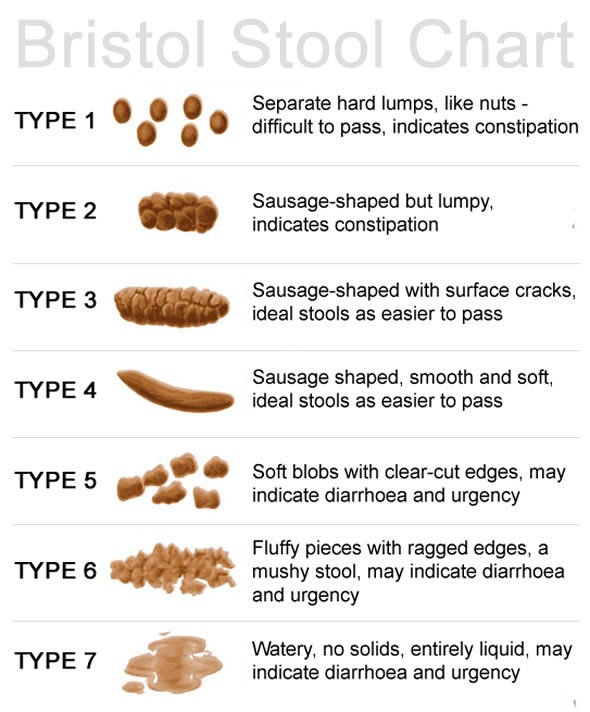
The stool consistency and type is noted and classified according to the Bristol stool chart. This helps determine the colonic transit time. Type 1 stool in the takes about 100 hours (slow transit) while Type 7 takes approximately 10 hours (rapid transit).
Investigations for diagnosis of underlying conditions include full blood count to exclude anaemia and thyroid function test to exclude hypothyroidism.
Imaging studies are used to rule out obstruction leading to constipation. Some of the imaging studies include air contrast barium enema that can help detect an obstructing colon cancer, intermittent volvulus, or colonic stricture.
Dynamic pelvic magnetic resonance imaging (MRI) helps in assessment of the anatomy during defaecation and therefore may identify pelvic floor dysfunction.
Other tests include Lower Gastrointestinal (GI)endoscopy, anorectal manometry, electromyography and defaecography.
Management of constipation in elderly
The aims of management of chronic constipation in the elderly are to restore normal bowel habits and ensure passage of soft, formed stool at least three times a week, without straining, and to improve the quality of life with minimal side effects.
Lifestyle changes include increased physical activity, eating a healthy and balanced diet with adequate fibers and fluids. There should be reduction in consumption of coffee, tea and alcohol as much as possible, and patients should consume extra glass of water for every drink of coffee, tea or alcohol.
Bowel training is also an important measure. The optimal times to have a bowel movement are soon after waking and soon after meals, when colonic transit is greatest. Patients are taught to recognize and promptly respond to the urge to pass stools. Failure to do so can result in a build up of stools and constipation. Patients are advised to adopt a “semisquatting” position to defecate. This could be achieved by using a footstool and leaning forward on the toilet.
Apart from fibers in foods patients are advised to take fibre/bulk supplements Psyllium (ispaghula husk), methylcellulose, polycarbophil, or bran.
Medications include osmotic laxatives, stimulant laxatives, and other agents. Bulk laxatives include Psyllium (ispaghula husk), methylcellulose, polycarbophil, bran.
Osmotic laxatives include lactulose, sorbitol, mannitol, salts of magnesia, sulphate, phosphate, polyethylene glycol.
Stimulant laxatives include Senna, cascara and Diphenlmethane derivatives include bisacodyl.
There are enemas, liquid paraffin, phosphates, lubricants for fecal impaction as well.
Other options include sacral nerve stimulation, biofeedback system and surgery for refractory and severe cases.
Sources
- http://wwww.cfps.org.sg/sfp/35/353/353_original_paper1.pdf
- http://www.wjgnet.com/1007-9327/14/2631.pdf
- www.movicol.com.au/…/IMPACT%20for%20older%20patient.pdf
- www.cnca.ca/…/…n_of_Constipation_in_the_Older_Adult_Population.pdf
- www.med.umich.edu/bowelcontrol/patient/teaching/umconstipation.pdf
- www.gastro.org/…/AGAPatientBrochure_Constipation.pdf
Further Reading
- All Constipation Content
- What is Constipation?
- Constipation Diagnosis
- Causes of Constipation
- Constipation Treatments
Last Updated: Jun 20, 2019

Written by
Dr. Ananya Mandal
Dr. Ananya Mandal is a doctor by profession, lecturer by vocation and a medical writer by passion. She specialized in Clinical Pharmacology after her bachelor's (MBBS). For her, health communication is not just writing complicated reviews for professionals but making medical knowledge understandable and available to the general public as well.
Source: Read Full Article



