The coronavirus disease 2019 (COVID-19) has been thought to spread primarily when an infected person coughs or sneezes, but little is known about its transmissibility through activities such as breathing, talking and singing.
A new study led by researchers from the National University of Singapore (NUS), and conducted at the National Centre for Infectious Diseases (NCID), revealed that severe acute respiratory syndrome coronavirus (SARS-CoV-2) particles can be aerosolised by an infected person during talking and singing. They also found that fine aerosols (less than 5 micrometers, or μm) generated from these two types of activities contain more viral particles than coarse aerosols (more than 5 μm). The researchers concluded that fine respiratory aerosols may play a significant role in SARS-CoV-2 transmission, especially in an indoor environment, and hence, should be taken into consideration when planning infection prevention measures.
“While previous studies have established the relative amount of aerosols (or the amount of particles) produced through similar activities, they did not measure the amount of SARS-CoV-2 virus particles generated. To our knowledge, this is the first study to quantify and compare SARS-CoV-2 particles in aerosols generated through breathing, talking and singing. Therefore, our team’s work provides a foundation for estimating the risk of transmission of infection,” said project leader Associate Professor Tham Kwok Wai, who is from the Department of the Built Environment at the NUS School of Design and Environment.
The study was first published online in the journal Clinical Infectious Diseases on 6 August 2021. Within a day of its publication, the paper was ranked among the top 5 percent of all research outputs scored by data science company Altmetric, and was given one of the highest attention score after different factors, like the relative reach from social media sites, blogs, policy documents, and more, were taken into account.
Measuring SARS-CoV-2 particles in respiratory aerosols
The study involved 22 COVID-19 positive patients who were admitted to the NCID from February to April 2021. The NCID was the research site that selected and recruited the patients, and performed whole genome sequencing to determine their viral strains of infection.
The participants had to perform three separate expiratory activities on the same day. These activities involved 30 minutes of breathing, 15 minutes of talking in the form of reading aloud passages from a children’s book, and 15 minutes of singing different songs, with rest between activities.
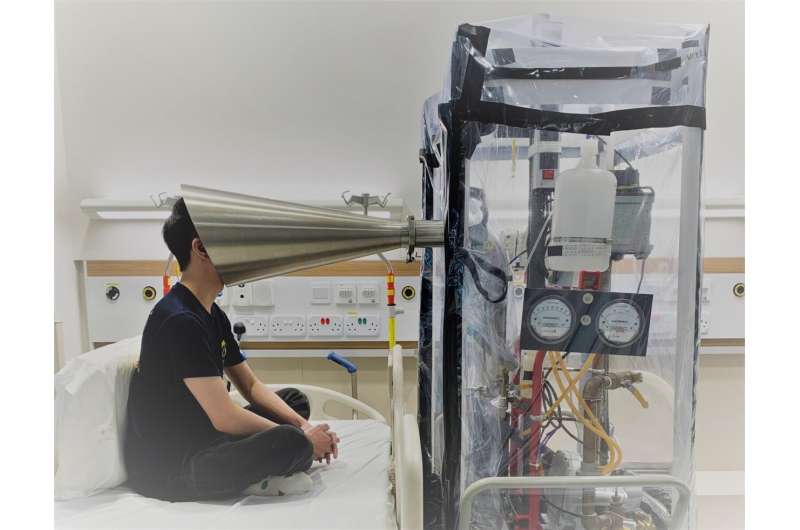
The participants had to carry out these three activities using a specially designed exhalation collection equipment known as the Gesundheit-II. This equipment was made available for this research by its inventor Professor Donald Milton from the University of Maryland, who is one of the co-authors of the paper and a collaborator on the project. In the studies, participants were required to place their head at the cone-shaped inlet of the equipment. This cone served as a ventilation hood where air is continuously drawn around the participant’s head, allowing the collection of expiratory particles into the connecting sampler.
Aerosols were collected in two size fractions, namely coarse (more than 5 μm) and fine (less or equal to 5 μm). The sample viral load was quantified by using a method known as reverse transcription-quantitative polymerase chain reaction.
“We observed that COVID-19 patients who are early in the course of illness are likely to shed detectable levels of SARS-CoV-2 RNA in respiratory aerosols. However, person-to-person variation in virus emission was high. Some patients surprisingly released more virus from talking than singing,” shared project co-leader Dr. Kristen Coleman from Duke-NUS Medical School.
“It has thus far been difficult to directly show how SARS-CoV-2 can be transmitted. Through the coordinating efforts of one of our resident doctors, Dr. Sean Ong, and the support of our nursing team and patients, we were able to study key high risk activities like talking and singing while ensuring the safety of the patients and staff involved. The end result provides direct measurements to show that besides respiratory droplets, virus particles emitted in exhaled breath and vocalization activities are likely important mechanisms for transmitting SARS-CoV-2,” said Dr. Mark Chen, Head, NCID Research Office, National Centre for Infectious Diseases.
The research also involved collaborators from the NUS Yong Loo Lin School of Medicine’s Departments of Microbiology and Immunology, Otolaryngology, and Medicine, Tan Tock Seng Hospital, National University Health System, as well as the Institute of Molecular and Cell Biology at the Agency for Science, Technology and Research (A*STAR). It was supported by the Singapore National Medical Research Council and NUS.
Multi-layered approach for infection control
The findings of this study demonstrated that exposure to fine-particle aerosols needs to be mitigated, especially in indoor environments where airborne transmission of SARS-CoV-2 is most likely to occur. Reducing exposure to fine respiratory aerosols can be achieved through non-pharmaceutical interventions, such as universal masking, physical distancing, increased room ventilation, more efficient filtration and appropriately applied air-cleaning technologies.
In particular, the research team recommended a multi-layered approach of control measures to decrease the risk of airborne SARS-CoV-2 transmission.
“Although our attempts to grow infectious virus in cell culture were unsuccessful, our studies can provide an important baseline to guide infection prevention activities,” explained Professor Paul Tambyah from the NUS Yong Loo Lin School of Medicine, who is one of the co-authors of the research paper.
“In situations involving singing, safe distancing among singers, as well as the averting and filtering of airflow from choir to audience, such as by deploying air curtains, are important considerations. For situations involving talking, determining airflow patterns and minimizing exposure through seating and furniture configurations, distancing, and air movement alteration, such as fans, including desk fans are practical options that can be taken to lower the risk of SARS-CoV-2 transmission,” commented Assoc Prof Tham.
Further studies
In view of more recent variants of the coronavirus, especially the Delta variant which has been reported to be more infectious, the researchers plan to use the same methods to determine if the aerosol viral load associated with the new variants, especially the Delta variant, is higher than previous strains.
Source: Read Full Article



