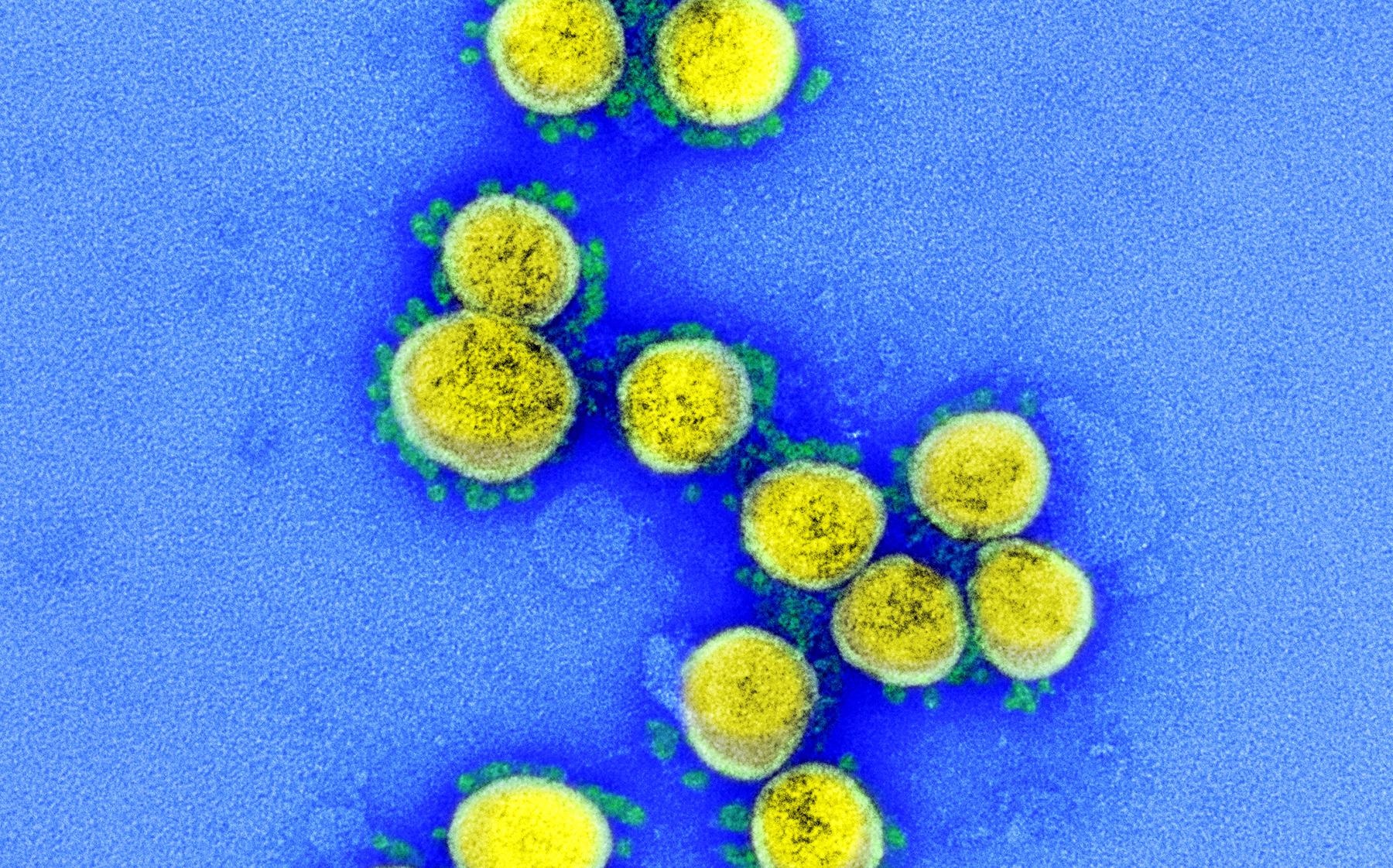
Natural immunity plays a critical role in protecting us from the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the pathogen responsible for coronavirus disease 2019 (COVID-19).
Interferons (IFNs) constitute a significant part of the anti-viral innate defense system. To establish an infection, SARS-CoV-2 needs to cross this defense mechanism of interferons.
The molecular patterns of viral pathogens are recognized by pattern recognition receptors which leads to the activation of signal cascades. This causes the induction and secretion of IFNs as well as other pro-inflammatory cytokines.
Further, these secreted IFNs bind to their respective receptors, which leads to the induction and expression of several interferons stimulated genes (ISGs).
Interferons are categorized into three types: Human type I IFNs (includes IFNα and IFNβ), Type II IFNs (includes IFNγ), and Type III IFN (includes IFNλ1-4).
Due to the continuous adaptation of SARS-CoV-2 to the human population, multiple variants of concerns (VOCs) have emerged with increased infectiousness and decreased sensitivity to preventive or therapeutic measures.
The World Health Organization (WHO) has classified four SARS-CoV-2 variants as VOCs: B.1.1.7, B.1.351, P.1, and B.1.617.2. These are also known as alpha, beta, gamma, and delta variants, respectively.
Comparing the replication efficiency of SARS-CoV-2 variants of concerns with the early isolate of SARS-CoV-2
In a study recently published on the bioRxiv* preprint server, researchers investigated the difference in replication efficiency or IFN sensitivity of the four VOCs.
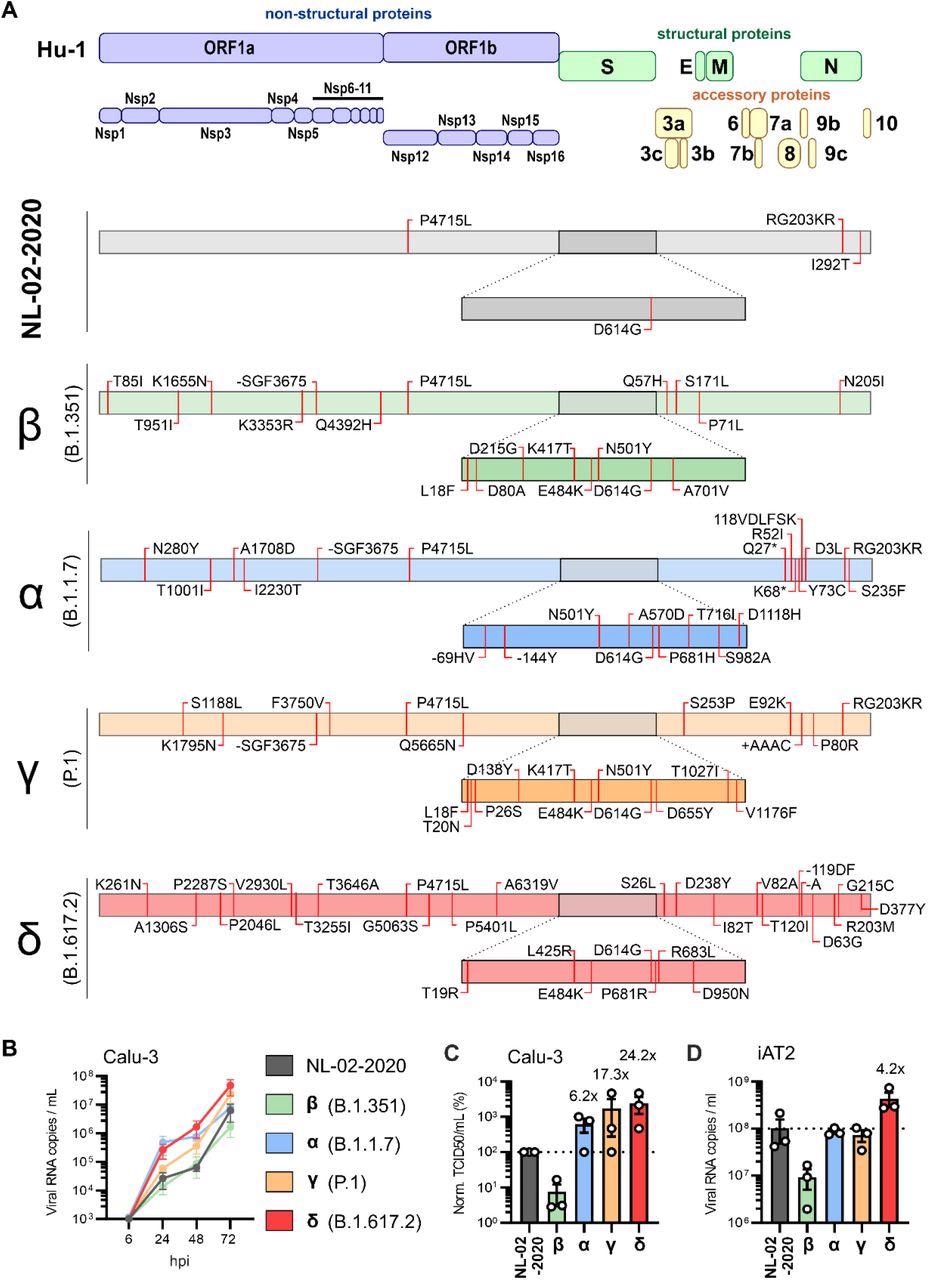
Since the first available sequence of the Wuhan-Hu-1 isolate, mutations were observed in the S glycoprotein, proteins involved in replication, and innate immune escape of SARS-CoV-2 isolate from February 2020 (NL-02- 2020) and four VOC isolates.
In this study, the researchers utilized the human epithelial lung cancer cell line Calu-3 and found that as compared to the NL-02-2020 isolate, the Delta variant replicated with greater efficiency.
Also, the SARS-CoV-2 alpha and gamma variants depicted intermediate phenotypes, whereas the SARS-CoV-2 beta variant replicated with moderately reduced efficiency compared to NL-02-2020.
The iPSC-derived alveolar epithelial type II (iAT2) cells comprise a major part of pulmonary alveolar epithelial cells and are considered the main targets of SARS-CoV-2 in the distal lung.
The researchers observed that compared to other SARS-CoV-2 isolates, the SARS-CoV-2 beta variant replicated with moderately reduced efficiency in the iAT2 cells.
With the increase in virus-induced loss of AT2 cells, the severity of COVID-19 also increases. The results showed that the sensitivity of NL-02-2020 isolate was more towards IFNβ, IFNγ, and IFNλ1 than toward IFNα2 in Calu-3 cells.
Also, it was demonstrated that in the presence of different concentrations of IFNs, the SARS-CoV-2 alpha variant showed the highest resistance against IFN treatment.
The SARS-CoV-2 delta variant was at least as sensitive towards IFN treatment as the NL-02-2020 isolate.
Furthermore, as compared in Calu-3 cells, type II IFN was less effective against SARS-CoV-2 in iAT2 cells. The SARS-CoV-2 alpha variant was the least vulnerable to IFNs, and the SARS-CoV-2 alpha, beta, and gamma variants show higher resistance against type III IFN. The SARS-CoV-2 delta variant remains as sensitive to IFNs as early 2020 SARS-CoV-2 isolates.
“The Alpha variant shows reduced susceptibility to IFNs.”
Findings could help improve IFN therapies against SARS-CoV-2 delta VOC
The emergence of SARS-CoV-2 VOCs could be attributed to various features like replication efficiency, the efficiency of immune evasion, and virion infectivity.
The combination of the Alpha variant’s IFN resistance and the increased replication fitness of the Delta variant poses an increased risk for the emergence of a new VOC which can be more harmful than existing VOCs.
The deletion in Nsp6 has been found to be a shared trait among SARS-CoV-2 alpha and gamma VOCs with reduced sensitivity to type III IFN.
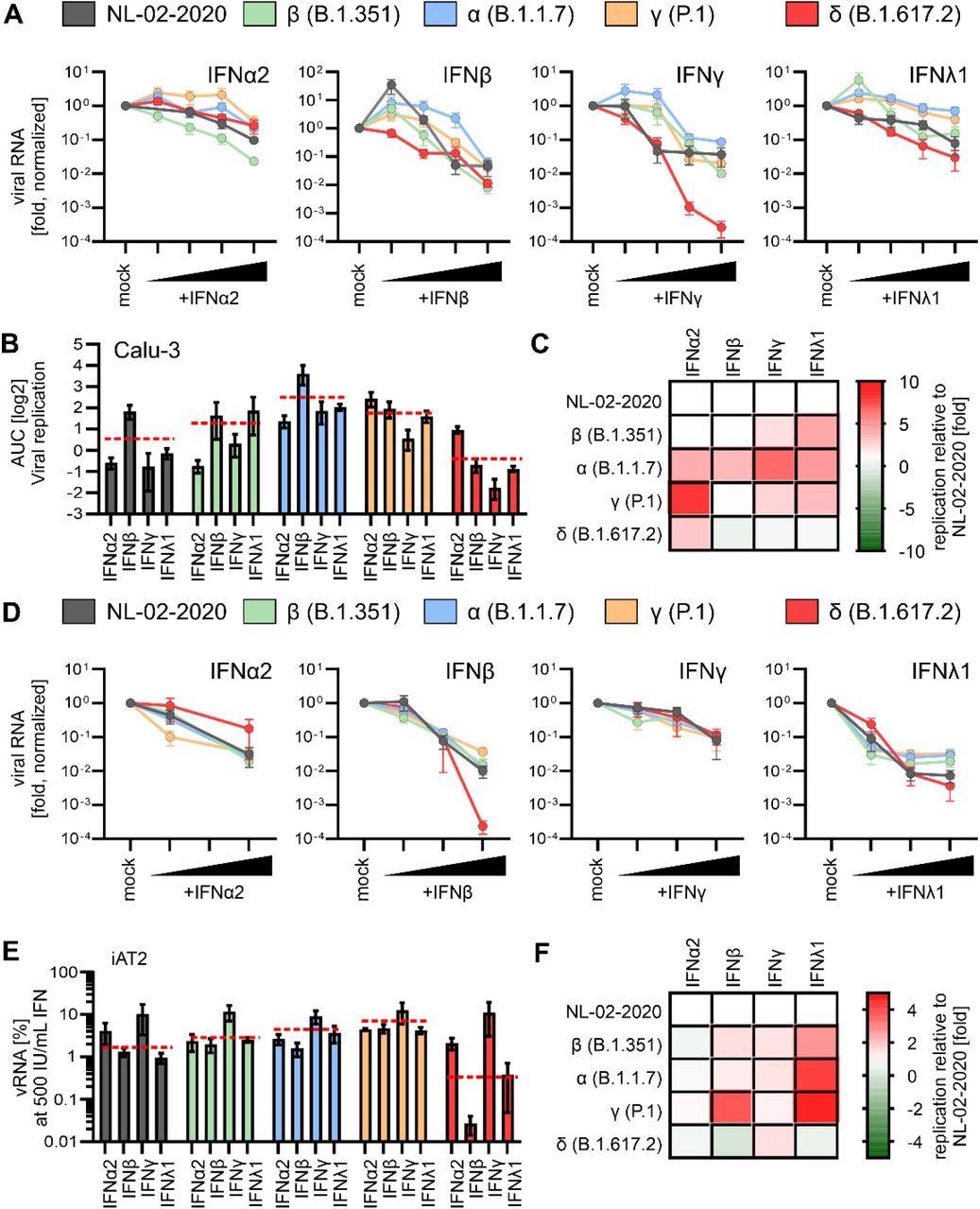
The study results show that IFNβ and IFNλ1 effectively inhibit the SARS-CoV-2 delta variant in human alveolar epithelial type II cells. This can help improve IFN-based therapies against the currently dominant SARS-CoV-2 delta VOC.
“Further studies on the molecular determinants of reduced IFN sensitivity and improved innate immune evasion of emerging SARS-CoV-2 variants are highly warranted.”
*Important Notice
bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- The Delta variant of SARS-CoV-2 maintains high sensitivity to interferons in human lung cells. Rayhane Nchioua, Annika Schundner, Dorota Kmiec, Caterina Prelli Bozzo, Fabian Zech, Lennart Koepke, Manfred Frick, Konstantin M. J. Sparrer, Frank Kirchhoff, bioRxiv, 2021. DOI: https://doi.org/10.1101/2021.11.17.468942, https://www.biorxiv.org/content/10.1101/2021.11.16.468777v1
Posted in: Medical Research News | Disease/Infection News
Tags: Amino Acid, Cancer, Cell, Cell Line, Coronavirus, Coronavirus Disease COVID-19, Cytokines, Genes, Genome, Genomic, Glycoprotein, immunity, Interferon, Interferons, Lung Cancer, Pathogen, Respiratory, RNA, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Syndrome, Virus

Written by
Saurabh Chaturvedi
Saurabh Chaturvedi is a freelance writer from Jaipur, India. He is a gold medalist in Masters in Pharmaceutical Chemistry and has extensive experience in medical writing. He is passionate about reading and enjoys watching sci-fi movies.
Source: Read Full Article



