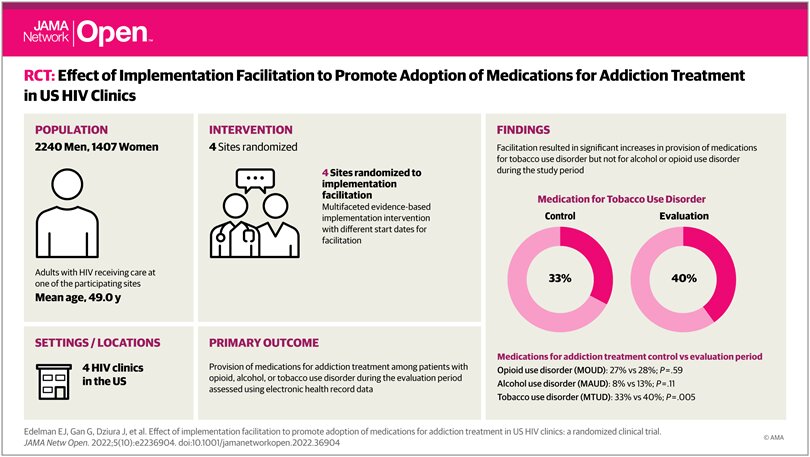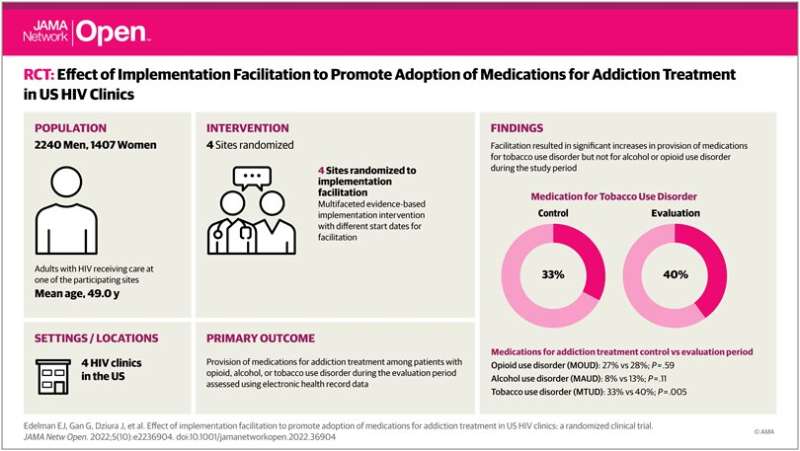
Given the benefits of antiretroviral treatment, for many individuals with HIV, substance use disorder—including opioid, alcohol, and tobacco use disorder—is a greater threat to their health than the virus. Although medications and behavioral treatments are available to address these conditions, many patients are not offered them and do not have the opportunity to benefit.
In collaboration with four partnering HIV clinics in the US northeast and in the context of the New England HIV Implementation Science Network, a group of Yale School of Medicine doctors led a randomized clinical trial to evaluate the impact of Implementation Facilitation, a package of implementation strategies (e.g., learning collaboration, external facilitation, education and academic detailing), to help clinicians and staff at these sites enhance provision of proven addiction treatments to their patients.
The results of this new study published in the journal JAMA Network Open show these efforts have made some headway in promoting receipt of medications for alcohol and tobacco use disorder, but the investigators did not see much improvement in delivery or receipt of medications for opioid use disorder.
“It was exciting to see that we’ve moved the needle in some areas, but there are still gaps in treatments for these patients who have life-threatening conditions,” said E. Jennifer Edelman, MD, MHS, associate professor of medicine and of public health and lead author of the study.
The team led by Edelman and senior author David Fiellin, MD, professor of medicine, of emergency medicine, and of public health and director of the Yale Program in Addiction Medicine, provided clinicians and staff at four HIV clinics in the northeastern United States with expert advice from addiction specialists about medication and counseling treatments to combat addictions and strategies to ensure patients receive care for substance use disorders.
Source: Read Full Article