Recent research from CU Boulder may have finally revealed why humans tend to get sick from airborne viral diseases more often in drier environments.
Published in December in PNAS-Nexus, the study found that airborne particles carrying a mammalian coronavirus closely related to the virus which causes COVID-19 remain infectious for twice as long in drier air, in part because the saliva emitted with them serves as a protective barrier around the virus, especially at low humidity levels.
The study carries major implications for not only the current COVID-19 pandemic but potentially for all infectious diseases transmitted by saliva-coated viruses. The research also further emphasizes the importance of managing indoor air filtration and ventilation to mitigate airborne disease spread, especially for buildings in arid states such as Colorado, dry enclosed environments such as airplane cabins and during dry winter months in temperate climates worldwide.
“The physics of the air in our buildings and the climate in which we live affect things that can make us sick and how long they persist. Now we have conservative indications of how long coronaviruses like the one that causes COVID-19 can stick around in the air and be an infectious disease threat,” said Mark Hernandez, senior author and S. J. Archuleta Professor of Civil and Environmental Engineering.
In 2020, Hernandez had a hunch that both relative humidity and saliva were important factors in the transmission of the novel virus sweeping the globe. He also happened to run the Environmental Engineering Microbiology and Disinfection Lab, one of the country’s only full-scale bioaerosol labs ready and able to take on the challenge at the start of the pandemic.
Civil engineers design and operate buildings in the U.S. to maintain an indoor relative humidity between about 40% and 60%. In the real world, however, these percentages vary more widely. In San Francisco for example, where Hernandez grew up, the relative humidity pushes a dewy 60%. In comparison, Colorado hovers at an arid 25%.
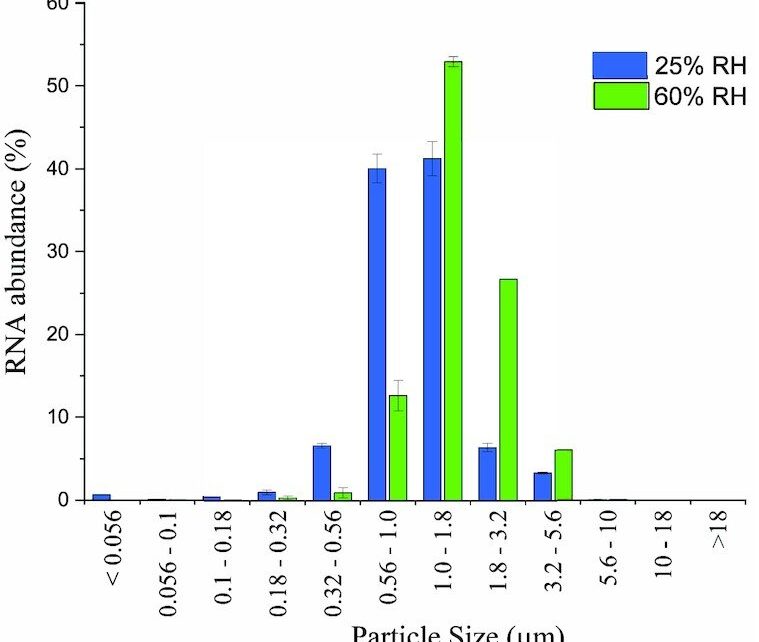
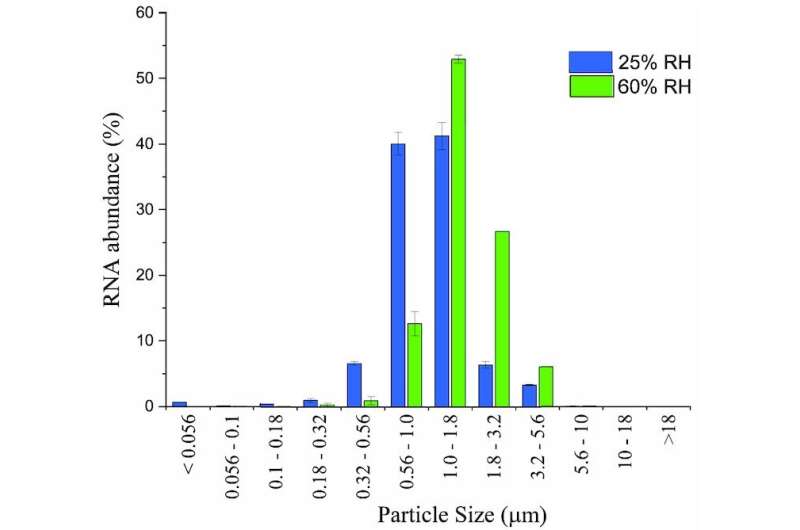
So they released virus-laden, airborne particles into several state-of-the-art, sealed chambers—the largest one about the size of a large bathroom—both with and without saliva, and at 25%, 40% and 60% relative humidity.
They found the saliva acted as a protective mechanism for the virus regardless of the humidity level. At both 40% and 60% relative humidity, half of the airborne coronavirus particles were still infectious after aging for one hour in the chamber. But at 25% humidity, that time doubled: Half of the original particles released into the chamber remained infectious for two hours.
“It shows this virus can hang around for quite a while—hours, even. It’s longer than a class, longer than the time you’re in a restaurant, longer than the time you take to hang out in the cafe. An occupant may come in, spread coronavirus in the air, and leave. Depending on architectural factors, then someone else could walk into that space with potent doses still hanging around,” said Hernandez.
As the virus can remain infectious in the air longer than it takes most ventilation systems to remove it, additional air-focused mitigation measures such as filtration are required to reduce transmission, the study suggests.
“I hope this paper has an engineering impact in our buildings, for example, in schools and hospitals, so we can minimize the infectivity of these viruses in the air,” said Marina Nieto-Caballero, lead author, who earned her doctorate in the Hernandez bioaerosol lab in 2021 and is now a postdoctoral researcher at Colorado State University.
Using saliva for science
Temperature, light and relative humidity can all affect how long a viral particle remains infectious, but until now, no study had accounted for the fluids that carry them. Yet people are always producing saliva and emitting tiny particles into the air every time they talk, laugh or even sing, said Hernandez.
The team used medical-grade fake saliva to mimic those particles and turned to chemistry professor Magaret Tolbert to examine samples of saliva-protected virus under a typical microscope on flat plates, as well as with a special microscope that measures them in air.
Together, they found it’s not the proteins in saliva—as hypothesized by other scientists—that allow the virus to persist so well in drier air, but its sugary carbohydrates that stabilize them. While many types of airborne particles, such as common salt particles, crystallize in lower relative humidity, the saliva particles became gelatinous, even glassy, said Tolbert.
The researchers suspect it is this physical state, somewhere between solid and liquid, that provides the virus extra protection and allows it to linger longer in dry air.
Hernandez hopes the findings can help open the door for more “messy” research using more realistic scenarios to better understand airborne particles.
“Let’s get more real about how we test things in the lab. Let’s use saliva. Let’s use lung fluids. Let’s use blood. It’s scary, and it’s more expensive. But without that data, we don’t know,” said Hernandez
Research in dry climates, for dry climates
Coloradans are among the 100 million Americans who live in a dry climate and who could, as a result, be at increased exposure risk indoors for airborne viruses such as coronavirus.
While more research is needed, this study could partially explain why Colorado was one of 16 states with a “very high” rate of influenza-like illnesses last November, according to data from the Centers for Disease Control and Prevention.
But what can those of us who live or spend time in drier environments do?
While it may be worth increasing relative humidity indoors to at least 40%, humidifying indoor spaces is expensive and inefficient, said Hernandez.
“Instead, we can add simple, inexpensive air filters that will take particles out of the air faster. We can increase the ventilation rate, open windows, and make sure we get more fresh air through,” said Hernandez. “We’ve known this from the beginning, but this research gives us a target.”
More information:
Marina Nieto-Caballero et al, Carbohydrate vitrification in aerosolized saliva is associated with the humidity-dependent infectious potential of airborne coronavirus, PNAS Nexus (2022). DOI: 10.1093/pnasnexus/pgac301
Journal information:
PNAS Nexus
Source: Read Full Article