An international team of scientists has uncovered one of the mechanisms explaining how some leukemias evade treatment by changing their appearance and identity.
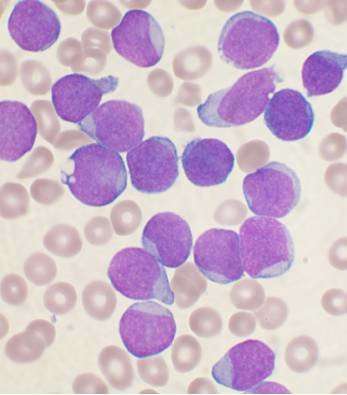
Most children with the common blood cancer B-cell acute lymphoblastic leukemia (ALL) have benefitted from huge improvements in treatment over the last 50 years and nine in every 10 children diagnosed will now be cured.
For those whose leukemia does not respond to treatment, much hope has been placed on new antibody and immune cell-based treatments, such as CAR T-cells, which specifically target the surface of leukemia cells.
Changing appearance
Doctors, however, have seen that some of these leukemias can evade immune therapies by stopping the production of the cell surface proteins which these therapies target, or even by switching to become a different type of cancer against which these new treatments are ineffective.
This is a particular problem for leukemias caused by genetic rearrangements involving a gene called MLL.
Teams from Newcastle University, U.K., the Princess Maxima Center in Utrecht and the University of Birmingham, have now revealed one of the mechanisms explaining how these chameleon cancers change their appearance and identity.
Publishing in the journal Blood, they have studied this cell identity switching behavior in leukemias caused by the MLL/AF4 fusion gene.
Dr. Simon Bomken, MRC Clinician Scientist and Honorary Consultant at Newcastle University and co-lead author of the paper, said, “ALL cells carrying this chromosomal rearrangement have long been known to be able to relapse as a different type of blood cancer, acute myeloid leukemia (AML). When this switch occurs, the leukemia becomes extremely difficult to treat.
“By studying MLL/AF4 leukemias we showed that the switch can happen in blood cells throughout different stages of development in the bone marrow.
“Importantly, the switch can be a result of additional genetic changes that can be caused by chemotherapy itself. As a consequence, some leukemias completely ‘re-program’ themselves and switch identity from one cell type to another.”
The team found that this re-programming can be driven by changes to master control genes, including CHD4 which is normally required to switch off the genes important for development of AML.
Important implications
Dr. Bomken, honorary consultant pediatric oncologist at Newcastle Hospitals, added, “These results have important implications for our understanding of disease development and response to therapy.
“They begin to enable us to identify which patients are at greatest risk of relapse, thereby informing the choice of which treatments to use and when.
Source: Read Full Article



