Conventional vaccines usually contain antigens—components of the respective pathogens—that bind to receptors on the surface of their target cells in order to trigger the disease. Scientists at the Berlin Institute of Health at Charité (BIH) and the Max Delbrück Center have now discovered that antigen variants with low receptor binding can be advantageous for the development of vaccines.
The research team has succeeded in producing a new vaccine against the SARS-CoV-2 coronavirus by identifying spike protein mutants that lack binding affinity. The scientists have now published their findings in the European Journal of Immunology.
Vaccines induce the production of specific neutralizing antibodies against the pathogen antigens administered into the body, such as the SARS-CoV-2 virus’s spike protein. If a subsequent infection occurs, these antibodies can be mobilized to fight against the pathogen. To achieve high vaccine efficacy, it is essential that sufficient amounts of pathogen components circulate in the blood after vaccination.
The number of pathogen components floating around freely in the blood is, however, reduced because they have the property of binding to receptors. Often, pathogens—and therefore the components of the inoculated pathogens, as well—find suitable receptors at many sites in the host organism to which they can dock.
This is also the case with the SARS-CoV-2 virus. The central role here is played by the ACE2 receptor, which interacts with the virus’s spike protein. This receptor is not only present in the respiratory tract, but is also widely distributed throughout the body. The spike protein can occupy ACE2 receptors in both COVID-19 infection and vaccination.
But Kathrin de la Rosa believes this is likely to be disadvantageous, particularly when it comes to the immune response. The immunologist holds the Johanna Quandt Professorship for Translational Immune Mechanisms at the BIH and also leads a research group at the Max Delbrück Center. “Once vaccine components have bound to suitable receptors on cell surfaces,” explains de la Rosa, “they are more or less protected from being attacked by the immune system.
“They provide B cells, which are responsible for producing pathogen-specific antibodies, with less of a target, because the receptor binding effectively masks the identifying feature from these immune cells. As a result, vaccine efficacy is reduced.”
And there may be another disadvantage: It cannot be ruled out that vaccine-induced receptor binding could lead to cellular malfunctions and a disturbance of balance within the body.
A clever bit of selection
In de la Rosa’s view, a vaccine should ideally be both “body inert” (barely reactive in the body) and “B-cell activating.” Out of this combination came the name BIBAX, which is what the researchers call the innovative type of vaccine they have developed and successfully tested against SARS-CoV-2. The spike protein served “merely” as a model protein, because—as was clear from the outset—the new strategy could also be of interest for other vaccines.
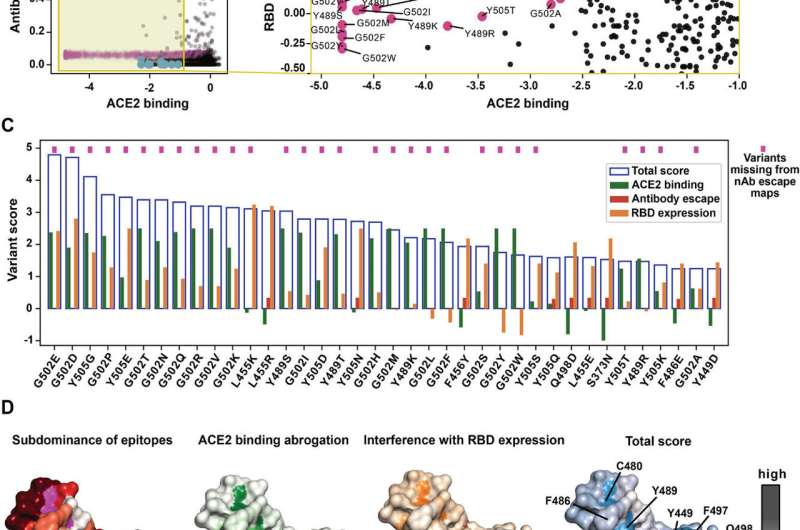
Variants that possess a low tendency to bind to receptors—in this case ACE2 receptors—should be advantageous for the development of vaccines, according to the scientists’ vision. Their work involves using various lab-made variants of the spike protein that each have slightly different functional properties as a result of point mutations (minute genetic changes).
Using an innovative computational approach, the researchers sifted through deep mutational scanning data for spike antigen mutants that lack binding affinity but have high immunogenicity. And they found one—called RBD-G502E—that was very close to the desired profile and selected it as the antigen variant for their vaccine.
A new vaccine prototype?
“Our studies in cell cultures and in animal models indicate the superiority of the novel SARS-CoV-2 vaccine, which we believe is suitable as a prototype,” explains de la Rosa, adding that she expects it to have a targeted, potent effect on B cells. “We demonstrated that the spike protein variant RDB-G502E hardly binds at all to the ACE2 receptor.”
Receptor transport to the cell interior, as would be typical after binding of the antigen to its receptor, was not observed when RDB-G502E was used.
This antigen variant also fulfilled expectations with regard to its immunogenicity. In rabbit immunizations, the RDB-G502E-based vaccine resulted in 3.3-fold higher concentrations of neutralizing antibodies in the blood compared to a conventional vaccine.
The chances of providing reliable vaccine protection against SARS-CoV-2 could be significantly improved by a targeted selection of immunogenic pathogen antigens that lack binding affinity. And de la Rosa’s group believes this new type of vaccine design also holds promise for fighting other pathogens.
“Effective vaccines are available for SARS-CoV-2, but they are lacking for other pathogens despite intensive research,” stresses de la Rosa. “We have preliminary evidence that the BIBAX strategy may be beneficial for vaccine protection against other coronaviruses and herpes viruses, against which adequate vaccine protection has not been achieved to date.” The team plans to investigate these findings further.
More information:
Christoph Ratswohl et al, A design strategy to generate a SARS‐CoV‐2 RBD vaccine that abrogates ACE2 binding and improves neutralizing antibody responses, European Journal of Immunology (2023). DOI: 10.1002/eji.202350408
Journal information:
European Journal of Immunology
Source: Read Full Article



