All the chairs in the waiting room were filled by dozens of newly arrived migrants waiting to be seen by a Cook County health worker at a clinic in Chicago. Julio Figuera, 43, was among them.
He didn’t want to talk much about traveling to Chicago from Venezuela, where a social, political and economic crisis has pushed millions into poverty and led 7 million to flee, Figuera and three of his kids included.
But somewhere along the way, he’d gotten pneumonia.
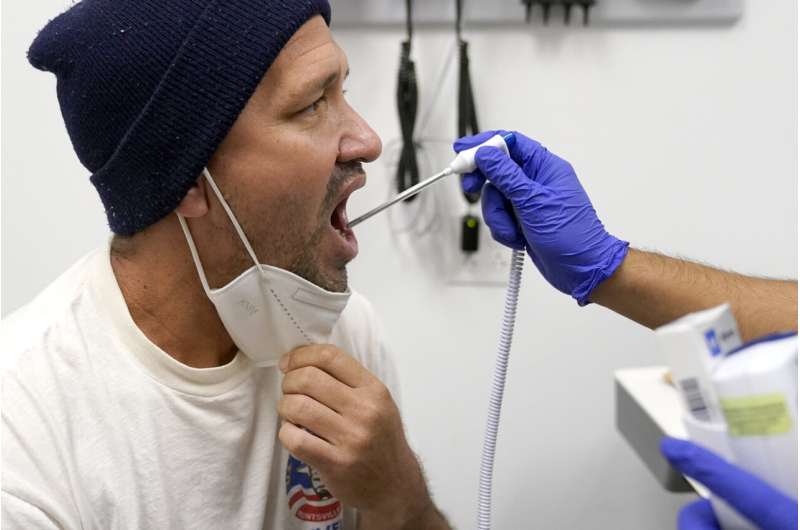
Figuera, who was living with hundreds of other asylum-seekers at O’Hare International Airport while waiting for more permanent shelter, returned for follow-up care at the county clinic. The stubborn cough came back, so he did, too. The staff checked his vitals, listened to his chest and gave him a hepatitis vaccine.
“I rarely get sick,” he said. “It was the journey that got me sick.”
Tens of thousands of migrants who’ve come to the United States are navigating a patchwork system to find treatment for new or chronic health concerns.
Doctors across the country say it’s rare that migrants receive medical screenings or anything beyond care for medical emergencies when they arrive at the U.S.-Mexico border, and there’s no overarching national system to track the care, either. Migrants’ options dwindle or expand after that—depending on where they end up—with some cities guiding new arrivals into robust public health systems and others relying on emergency departments or volunteer doctors to treat otherwise preventable health issues.

“You have these little islands of care. You have these little islands of shelter,” said Deliana Garcia, of the nonprofit Migrant Clinicians Network, which supported more than 1,000 migrants in need of medical care in the first 10 months of this year. “But how does anyone know what’s going on east to west or north to south?”
More than 2 million people crossed the border illegally between October 2022 and September 2023, according to Border Patrol data. For the most part, doctors told The Associated Press, the migrants are healthy; they have to be to make the arduous journey. It’s the travel that can turn manageable health issues into emergencies.
Because of that, public health leaders across the country—from New York to Los Angeles, Boston to Denver—say there’s high demand for care. And providing it is central to their organizations’ missions.
“It’s so core to what we do that I don’t feel like anyone’s really hesitated around this is the right thing for the organization to do,” said Craig Williams, chief administrative officer of Cook County’s health system. “I don’t feel like over the last year that we’ve backed off from really anything else because of doing this initiative.”

The cost of care
The work is not without a price: Roughly 14,500 migrants have visited the Cook County clinic this year, as many as 100 are picked up in vans from the shelters each day for immediate care, vaccinations and a foothold into the public health care system. The county spends about $2.2 million a month—or nearly $30 million since it opened the clinic about a year ago.
New York City Health and Hospitals logged 29,000 migrant patient visits in the last fiscal year, which ended in mid-June. There, health workers have administered more than 40,000 vaccines and provide medical screenings for all new arrivals.
Other cities are trying to manage as best they can, like Denver, where nearly 26,000 migrants have arrived within the last year. Dr. Steve Federico, a director at Denver Health, said the city’s process is inadequate.

Migrants are asked by shelter staff if they need immediate medical attention. If they say yes, they’re either sent to an emergency room or connected by phone with a nurse through Denver Health, a public hospital and health organization.
There are no basic health screenings, Federico said, which can increase the risk of infectious disease outbreaks among those living in shelters. In Chicago, one shelter saw a small outbreak of chickenpox.
Without catching and treating illnesses early, Federico said, “Now everybody has it. And then if somebody is at increased risk, they’re going to get sicker.”
Federico and city spokesperson Jon Ewing both said Denver is already strained for resources—given the need to shelter and feed migrants. Ewing said Denver is looking to enhance its medical screening process, but added that it’s not clear how much that will cost or whether there are enough resources to achieve it.

The challenges of care
Migrants face a lack of access to steady medical care in the U.S., as well as healthy food and stable housing. It can mean that someone with a chronic medical condition, like diabetes or hypertension, can end up in the hospital simply because they lost or ran out of their medications, or had them confiscated during their travels. Doctors said they’ve also seen migrant children with asthma who need new inhalers.
“You have what were essentially healthy people put in really remarkable circumstances, where they are not able to survive thoroughly and then they come across (the border) in a really compromised state,” said Garcia, of the Migrant Clinicians Network.
Some women are arriving far along in their pregnancies, and never had prenatal care.
“We gave the first prenatal visit to a woman who was nine months pregnant just two weeks ago,” said Dr. Ted Long, senior vice president at New York City Health and Hospitals, where more than 300 healthy babies have been born to migrant mothers.

Even when care is available, migrants can have a hard time getting it. Some avoid asking for help entirely out of fear of a large bill or longstanding distrust of the medical system.
Dr. Stephanie Lee is the medical director of refugee resettlement and coordinator of the unaccompanied youth program at Penn State Health’s Family Practice Pediatrics Clinic. She said she sees many patients who don’t have health insurance or don’t know how to get it.
One mother who’d been waiting on an asylum request for more than a year told Lee she was paying out of pocket because her family didn’t have insurance.
“The process is so broken that you can’t even do anything,” Lee said. “They came in to see me just paying out of pocket because the kiddo needed a physical and needed to get checked before going to school.”

The Migrant Clinicians Network, which has been connecting patients to health providers for 30 years, just received a $5 million grant from the National Institutes of Health. Its case workers keep in touch with migrants, doing things like setting up medical appointments, helping fill out applications for social services, taking people to appointments and figuring out payment options.
They even keep in touch with a trusted family member in the migrant’s home country, in case they fall off the radar.
“We have a lot of babies who are named after the people who work on our team,” said Garcia, who oversees the program.
But that’s the best-case scenario.
The shelter system in Massachusetts is so full that the governor brought in the National Guard in August to assist. Dr. Fiona Danaher and her colleagues often cannot find migrants when she needs to follow up because they don’t have a U.S. phone number.
-

Julio Figuera, 43, gestures as he talks about his life traveling to the U.S. from Venezuela and living at O’Hare International Airport while he waits for medical treatment at the Cook County, Ill., medical clinic on Monday, Oct. 16, 2023, in Chicago. Figuera, developed pneumonia since arriving in the U.S. and has been living with hundreds of other asylum seekers at the airport while awaiting more city permanent shelter. When migrants began arriving in Chicago last year, city leaders tapped the county’s health system to take over medical care. Credit: AP Photo/Charles Rex Arbogast
-

Julio Figuera, 43, receives a vaccine at the Cook County, Ill., medical clinic on Monday, Oct. 16, 2023, in Chicago. "I rarely get sick," he said. "It was the journey that got me sick." Figuera, developed pneumonia since arriving in the U.S. and has been living with hundreds of other asylum seekers at O’Hare International Airport while awaiting more city permanent shelter. When migrants began arriving in Chicago last year, city leaders tapped the county’s health system to take over medical care. Credit: AP Photo/Charles Rex Arbogast
-

Dr. Dan Vittum, one of the three doctors at the Cook County, Ill., health clinic, talks about the clinic’s mission in serving the immigration population arriving from the southern border on Monday, Oct. 16, 2023, in Chicago. "The bulk of the people who are coming through have had a traumatic experience, not only during the journey … but the reason why they left their homeland," said Vittum. Credit: AP Photo/Charles Rex Arbogast
-

Julio Figuera, 43, talks about his life traveling to the U.S. from Venezuela and living at O’Hare International Airport while he waits for medical treatment at the Cook County, Ill., medical clinic on Monday, Oct. 16, 2023, in Chicago."I rarely get sick," he said. "It was the journey that got me sick." Figuera, developed pneumonia since arriving in the U.S. and has been living with hundreds of other asylum seekers at the airport while awaiting more city permanent shelter. When migrants began arriving in Chicago last year, city leaders tapped the county’s health system to take over medical care. Credit: AP Photo/Charles Rex Arbogast
-
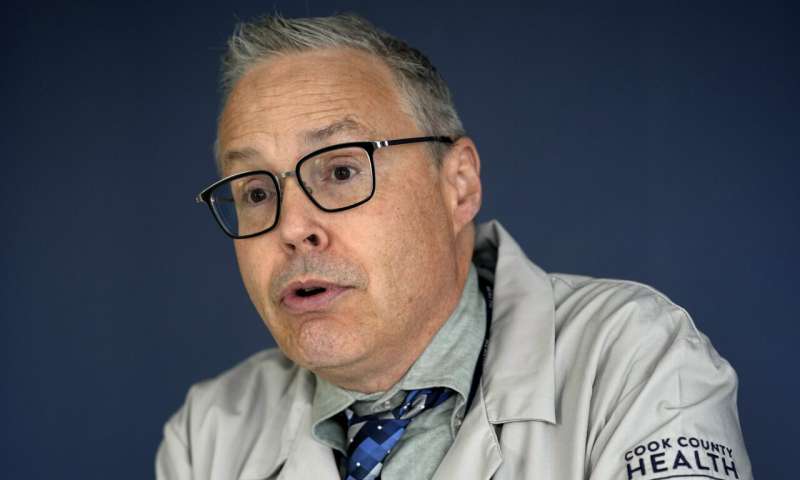
Dr. Dan Vittum, one of the three doctors at the Cook County, Ill., health clinic, talks about the clinic’s mission in serving the immigration population arriving from the southern border on Monday, Oct. 16, 2023, in Chicago. "The bulk of the people who are coming through have had a traumatic experience, not only during the journey … but the reason why they left their homeland," said Vittum. Credit: AP Photo/Charles Rex Arbogast
“We see situations even in migrants who are just moving around between shelter locations in the greater Boston area where they get completely lost to follow up,” said Danaher, a primary care pediatrician in the Mass General Brigham health system. “And then the wheel gets reinvented and the same tests get done.”
She encourages her colleagues to give patients a physical copy of everything that was done on their visit: vaccines administered, medications prescribed, benefit programs applied for. That way, they can simply hand it to whoever sees them next—like a critical game of telephone.
There’s “a lot of low hanging fruit” when it comes to caring for migrant patients, she said, and a “very old-school level of note passing” is “an important investment to make.”
© 2023 The Associated Press. All rights reserved. This material may not be published, broadcast, rewritten or redistributed without permission.
Source: Read Full Article



