Since 2008, we have known that the 16p11.2 chromosomal region is linked with autism spectrum disorder (ASD). Now, researchers from Boston Children’s have developed a new way to study the effects of 16p11.2 deletion in human neurons. In the process, they also found a potential treatment, possibly expanding the therapeutic options for this specific cause of ASD.
A common risk factor for ASD
Accounting for up to 1 percent of autism cases, deletions in 16p11.2—which includes 29 genes—occur in people who are missing a small amount of DNA on one copy of chromosome 16.
To better understand what happens in the brain cells of people with either deletions or additions of part of the 16p11.2 gene region, the researchers focused on a specific type called dopaminergic neurons. Defects in the dopaminergic system have been implicated in people with autism. Two drugs approved by the U.S. Food and Drug Administration to treat irritability associated with autism act on the dopaminergic system.
Measuring the activity of dopaminergic neurons
The work was done through a multi-institution collaboration co-led at Boston Children’s Hospital by Mustafa Sahin, MD, Ph.D., director of the Rosamund Stone Zander Translational Neuroscience Center and the Translational Research Program, and Christopher Walsh, MD, Ph.D., chief of the Division of Genetics and Genomics. Walsh was among the researchers who first discovered the association between 16p11.2 and ASD in 2008.
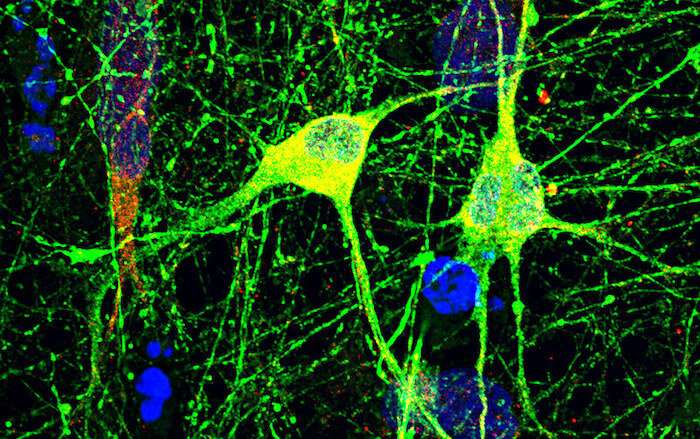
The team devised a way of differentiating induced pluripotent stem cells—created from patients’ own cells and bearing 16p11.2 copy number variations—into dopaminergic neurons. The investigators then studied how neurons missing the 16p11.2 region behaved in a dish.
“One advantage of making human stem-cell-derived neuronal cultures is that you can do drug testing very easily by measuring the activity of those cells,” explains first author Maria Sundberg, Ph.D., of the Sahin laboratory.
Their experiments involved probing the network activity of the derived dopaminergic neurons with more than 1,000 sensors at once. This allowed the team to observe how individual cells fired and then formed a cluster of signals that spread throughout the neuronal network in the dish.
“We discovered that dopaminergic neurons that are missing this 16p11.2 region were hyperactive compared to the control cells,” says Sahin.
Targeting the RhoA pathway
The team next used their culture technique to see if they could find pathways and drugs that calm the misfiring of the dopaminergic neuron cultures. Using information from earlier studies, the team focused on the KCTD13 gene in the 16p11.2 region, a gene known to regulate the RhoA pathway. RhoA is known to regulate nerve cell development.
Adding rhosin, a drug that specifically inhibits RhoA’s activity, slowed firing of the dopaminergic neurons with 16p11.2 deletions to a level equal to that of control cells.
“Rhosin essentially rescued the abnormal network activity of the 16p11.2-deletion neurons,” says Sundberg.
The specificity of this pathway raises the possibility of rhosin or similar inhibitors as potential treatment candidates, but their safety has not yet been studied in animal or human models of neurological disease.
“Our study demonstrates that the RHoA pathway plays an important role in the development of the network hyperactivity in these cells, and that inhibiting this pathway may be a potential new way to treat diseases like autism and neuropsychiatric disorders linked to 16p11.2 copy number variations,” says Sahin.
The team hopes to use this cell culture model to test FDA-approved compounds or other novel molecules in the future.
Source: Read Full Article



