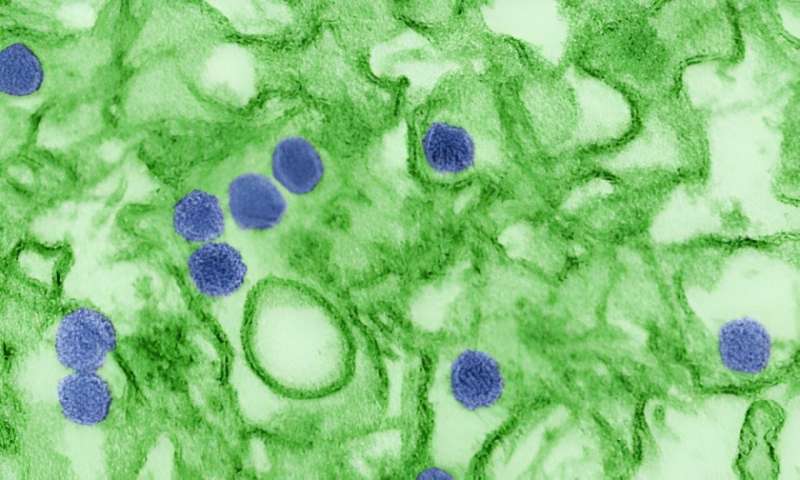
Before SARS-CoV-2 and COVID-19, there was the Zika virus epidemic, lasting from 2015 to 2016. The Zika virus can cause serious birth defects and abnormalities. During the epidemic, one of the most striking results of Zika virus in pregnant women was the increase in offspring suffering from microcephaly, a fetal growth restriction that can result in abnormal brain development.
While the Zika virus epidemic has ended, future outbreaks are inevitable as the majority of the world’s population lives in areas where the Zika virus mosquito thrives. Researchers in the Aagaard Lab at Baylor College of Medicine have studied how the virus persists in the placenta for long periods and how to mitigate it. Their findings are published in the American Journal of Obstetrics and Gynecology.
“At the maternal-fetal interface, there are immune niches and viruses that might take advantage of how long they are able to persist in the placenta,” said Dr. Enrico Barrozo, postdoctoral associate in the Department of Obstetrics and Gynecology at Baylor and first author of the paper.
Zika virus has a high maternal-fetal transmission rate leading to a number of fetal health issues, not just microcephaly. Infections can cause significant changes in early immune development. If a virus or microbe is able to persist for months, it can potentially have more of an effect on early immune development. Pregnant women infected with Zika virus have an increased chance of early pregnancy loss as well as a variety of other defects.
“The spectrum of babies isn’t just around microcephaly, but there are a number of different kinds of anomalies that can accompany Zika virus infection,” said Dr. Kjersti Aagaard, professor and maternal-fetal medicine expert in the Department of Obstetrics and Gynecology at Baylor and Texas Children’s Hospital. “They range from hearing loss to much more complicated and morbid conditions.”
Researchers used primary human placenta cells, a mouse fetal pathogenesis model and a new technology of spatial transcriptomics, which allows researchers to zoom in on placental microenvironments or niches. This is the first robust spatial transcriptomics study using mouse placenta. The study was conducted in three phases:
- First: used a primary human placenta subculture model to look at microRNA activity in response to Zika virus infection experimentally
- Second: studied Zika virus pathogenesis in a germ-free mouse model using enoxacin (formerly FDA-approved antibiotic) to look at the influence of microRNA networks on fetal pathogenesis
- Third: used spatial transcriptomics to detect differences in the placental immune microenvironments in the mouse model
The researchers zoomed in using spatial transcriptomics to identify potential effects of Zika virus infection on the placental microenvironments. Mice are usually resistant to Zika virus, but in this mouse model that did not have any live microbes, they were susceptible. Enoxacin is the only known way to increase microRNA activity.
Using this method, the researchers were able to rescue the fetal growth restriction caused by Zika virus, and Zika-associated transcriptional changes in the placenta were no longer observed in these mice.
“It’s really important to understand how viruses are—or are not—able to set up a niche in the placenta at the maternal-fetal interface,” Barrozo said. “We were very lucky to have this unique model where we had Zika virus susceptibility, and then we were able to untie the antibiotic part of enoxacin from its RNAi and microRNA activity.”
Moving forward, the research team hopes to uncover the parts of the microbiome that are associated with viral resistance and early immune development and when that occurs in pregnancy.
“Our next steps are continuing to develop an exciting new line of work around the animals that don’t have microbes (or gnotobiotic animals) and understanding why they are susceptible to Zika virus infection,” Aagaard said.
Other contributors to this work include Dr. Maxim Seferovic; Dr. Mark Hamilton; David Moorshead; Dr. Michael Jochum; Trang Do; Dr. Derek O’Neil; and Dr. Melissa Suter.
More information:
Enrico R. Barrozo et al, Zika virus co-opts miRNA networks to persist in placental niches detected by spatial transcriptomics, American Journal of Obstetrics and Gynecology (2023). DOI: 10.1016/j.ajog.2023.08.012
Journal information:
American Journal of Obstetrics and Gynecology
Source: Read Full Article