The statistics for pancreatic cancer are sobering. With a five-year survival rate of only 9%, incidence of the most common type, pancreatic ductal adenocarcinoma (PDAC), is growing and projected to be the second cause of cancer deaths by 2030. Surgery remains the most effective treatment, yet for 70-80% of patients, surgery is not a viable option. Understanding pancreatic cancer at the cellular and subcellular level is essential for developing therapies that can buy patients more time.
One way to extend survival is to optimize treatment strategy and to promptly switch strategies if treatment is not effective. Treatments may include a mix of radiation and chemotherapy. At present, assessing how well PDAC patients respond to this therapy typically relies on imaging and measuring blood serum levels of cancer biomarkers. However, both these methods come with drawbacks. Imaging (CT, MRI) cannot detect small tumors or differentiate benign from malignant ones, while the most well-established PDAC marker is not present in 5-20% of PDAC patients and can give unreliable results.
From garbage to gold
A study published today in Cells from the Systems Oncology Lab at Champalimaud Research provides a potential game-changer in how treatment response is assessed in PDAC patients.
Bruno Costa-Silva, principal investigator and the study’s senior author, first explored the potential of so-called “extracellular vesicles” (EVs) in fighting cancer in 2008. “EVs are tiny sacs released by cells. They’re like mini-cells, with a lipid membrane, genetic material, proteins and sugars. For a long time, they were dismissed as ‘trash bags,’ filled with waste products that cells wanted to throw out. But it’s now clear that they also transfer messages between cells.”
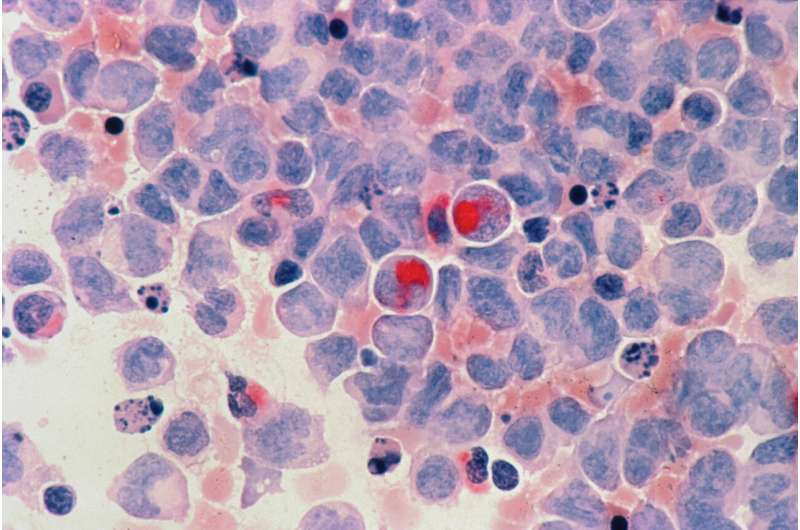
Given that plants and bacteria also release these small vesicles, EVs may be one of the most powerful forms of communication in living organisms. They are produced by virtually all cells, including cancerous ones. In fact, studies show that EVs secreted by malignant and non-malignant cells can contribute significantly to tumor progression.
In previous studies, Costa-Silva found that EVs in the blood may be used to detect, predict, and locate pancreatic cancer metastases. To date, though, researchers have been using one-off measurements of EVs in patients for either prognosis or diagnosis. “Ours is the first study to show that by looking at how EVs in pancreatic cancer patients change over time, we can tell how well they are responding to therapy,” says Costa-Silva.
From idea to discovery
When Nuno Couto, oncologist at the Champalimaud Foundation and the study’s lead author, began investigating the potential of EVs for monitoring treatment response, the team found a surprising result. “At first, we thought it was an artifact,” says Couto. “But it soon became clear that EVs in PDAC patients had significantly higher levels of a specific protein compared to EVs in healthy controls.” That protein was immunoglobulin G (IgG), a type of molecule that is part of our defense system, and which finds and kills foreign pathogens and cancer cells.
“The next step was the most challenging,” Couto admits. “In order to see how levels of these IgG-positive EVs in patients change during the course of treatment, we had to collect 20-30 blood samples from the same patient over many months. Without the help of the patients, nurses, clinicians, and pathologists at the Champalimaud Clinical Centre, this study would simply not have been possible.”
Using a special method developed by Costa-Silva’s lab to rapidly measure EV populations in tiny samples of blood, the team found that IgG-positive EVs increase during disease progression and decrease in response to therapy. As a result, these EVs represent a new biomarker that expands the repertoire of tools available to evaluate the tumor’s status, especially for the many patients that do not express the current standard biomarker, and for whom imaging is the only treatment response indicator.
“We were very excited to see such a close correlation between these vesicles and therapy response,” says Costa-Silva. “We now have a more reliable tool to assess, and improve, the efficacy of PDAC treatments, and to reduce the unnecessary and harmful side effects of ineffective ones.”
From oncology to cell biology
“This finding made me change the direction of my lab,” asserts Costa-Silva. “It’s impossible to look at these results, and not to think of immunology, or the broader implications for cell signaling.”
The researchers found that IgG binds to EVs in PDAC patients via a well-known cancer antigen. They suspect that EVs expressing this antigen are released by the cancer itself, so that IgGs become bound to the EVs instead of to their intended target: the tumor cells. In this way, the tumor would be able to evade the immune system’s arsenal, launching EVs to intercept IgG missiles.
“If very aggressive cancers like PDAC use EVs to disarm the immune system, we can develop new therapies to target tumor-derived EVs and make these cancers less resistant to treatment,” notes Costa-Silva. His team is now investigating whether proteins expressed by EVs in other cancer types also interact with molecules of the immune system.
As Costa-Silva puts it, “This is really about cell physiology. Cancers may use EVs to disrupt immunity, but EVs perform critical functions in non-cancerous settings too. Once released by a cell, proteins on the surface of EVs interact with other proteins and regulate their ability to interact with cellular targets, causing a cascade of knock-on effects in other cells. We’re very interested in learning more about these post-secretion interactions, and how EVs function as regulators of cell signaling.”
Source: Read Full Article



