A new CAMH study published in the journal JAMA Psychiatry found elevated levels of inflammation in the brain of patients who report persistent symptoms of long COVID.
Using advanced brain scanning with positron emission tomography (PET) imaging agents developed exclusively by the CAMH Brain Health Imaging Centre, study senior author Dr. Jeffrey Meyer and his study team found elevated levels of the protein TSPO, a brain marker of inflammation, in patients with onset of depression within several months after a COVID-19 infection.
“We already knew that there is brain inflammation in people who died in the midst of a severe, active COVID-19 infection. What’s new about this study is that it shows that inflammation is hanging around for a long time in the brains of people with long COVID even after only mild to moderate symptoms of active COVID-19,” said Dr. Meyer, Head of the Neuroimaging Program in Mood & Anxiety at the Campbell Family Mental Health Research Institute at CAMH.
“Inflammation in the brain was suspected of being the critical step in causing neurological and psychiatric symptoms of long COVID so confirming this is vital to develop treatments for people experiencing symptoms.”
It is generally believed that the majority of the world’s population has experienced at least one acute episode of COVID-19, and that at least 5 percent of those people—more than 200 million globally—may experience lingering neurological symptoms, including depression, loss of enjoyment, memory impairment, slower motor control, low motivation and energy, for months to even years due to brain inflammation from long COVID.
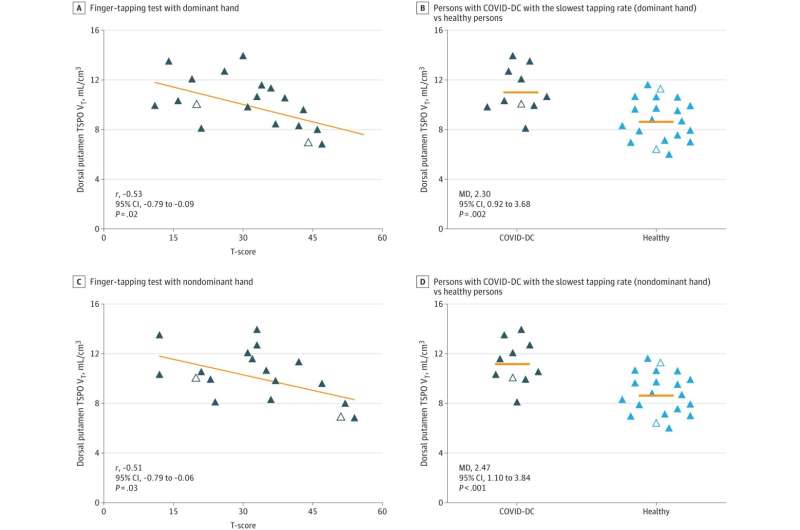
As part of this study, 20 participants underwent brain scanning with specialized PET imaging designed to detect the presence of elevated levels of the TSPO protein. All had at least one documented acute episode of COVID-19 after which they reported symptoms of depression that continued for months. Most participants also experienced a variety of other lingering symptoms associated with long COVID, including extreme fatigue and problems with concentration and memory often referred to as ‘brain fog’.
“What’s also noteworthy is that the regions of the brain that had the most inflammation are the ones involved in the capacity to enjoy things, motivational energy and the ability to think and move quickly. These were often the symptoms of greatest concern among the people with long COVID who took part in the study,” added Dr. Meyer.
In a pioneering 2015 study published in JAMA Psychiatry, Dr. Meyer found that the brains of people with depression had more inflammation—30 percent more on average—than the brains of people who were not depressed.
The greater the inflammation, the more severe the depression. It was the first time an association between depression and brain inflammation had been found. This research was so ground-breaking that it became one of the most highly cited international research studies ever produced to date by CAMH.
Dr. Meyer and his team believe that further study of the association between brain inflammation and depression, as well as further study on the short and long-term impacts of COVID-19 on the brain, could lead to new treatments for long COVID that would also be purposed for depression and other illnesses.
“For people who have been suffering from long COVID with lingering symptoms of depression, the hope is that we can use anti-inflammatory medications to see if we can get a reduction in symptoms,” said study first author Dr. Joeffre Braga. “Since inflammation can be in response to injury, it might also give us insight into mechanisms of brain injury in neurodegenerative diseases like Parkinson’s and prompt therapeutic development.”
More information:
Joeffre Braga et al, Neuroinflammation After COVID-19 With Persistent Depressive and Cognitive Symptoms, JAMA Psychiatry (2023). DOI: 10.1001/jamapsychiatry.2023.1321
Journal information:
JAMA Psychiatry
Source: Read Full Article



