It has been described as a stealth killer that impacts at least one in four Australians and is rising rapidly. Disease prevalence is expected to increase by 25–50% over the next 10 years, including 15–20% in children. It is a risk factor for cardiovascular disease, type 2 diabetes and a common type of liver cancer, and it is expected to become the leading cause of liver transplant within the next 20 years. So why have so few Australians heard of metabolic associated fatty liver disease (MAFLD), the most common cause of liver disease?
Well, it recently underwent a name change and this might be one reason. It used to be known as non-alcoholic fatty liver disease (NAFLD) but with advances in current knowledge of fatty liver diseases, it became apparent that the four-decade-old term could no longer be used to describe a disease with several root causes. The disease, as we understand it today, not only impacts patients who consume alcohol and those who do not, but also potentially impacts all patients with any form of liver disease by acting as a disease modifier. The name change was touted as a game changer, but the wheels may not be turning fast enough.
Unfortunately, with our current understanding, we are poorly placed to curb the rising health impacts associated with this disease, which is exemplified by a number of key challenges. It is defined as excessive accumulation of fat in the liver of people without excessive alcohol intake. Managing obesity is critical to managing this disease. Currently, lifestyle intervention is the frontline treatment for both obesity and MAFLD however, only a small proportion of people successfully manage their condition with lifestyle alone. And not all people who are overweight have MAFLD—in fact, about 40% of people are not at all and adiposity here is not the main driver. Unfortunately, when it comes to diagnosis, few effective non-invasive diagnostic and prognostic tools exist for this disease.
Current blood tests for liver function are often insufficient to capture the majority of those with underlying MAFLD, and so many patients go undetected until disease progresses to a severe state.
Relatively cheap and contemporary scanning techniques such as FibroScan may have benefit in improving diagnosis in certain at risk populations—particularly in those with diabetes.
Early detection is critical to preventing subsequent complications, however more than 80% of patients with metabolic associated fatty liver disease have few symptoms and fail to visit their doctor until their disease has progressed to a stage that is mostly irreversible. As for treatment, there are currently no clinically approved pharmacological therapeutics that specifically treat this disease.
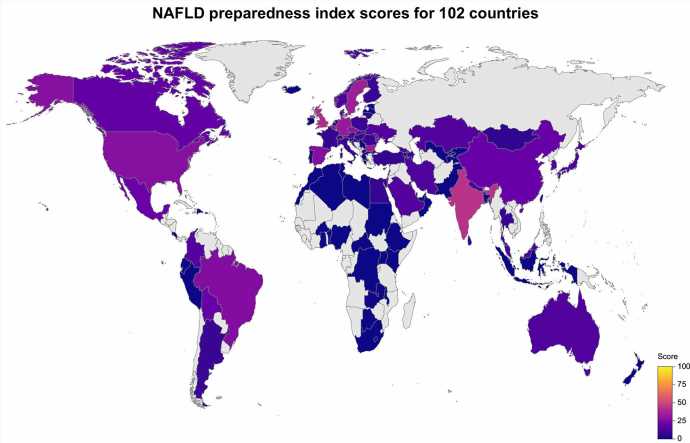
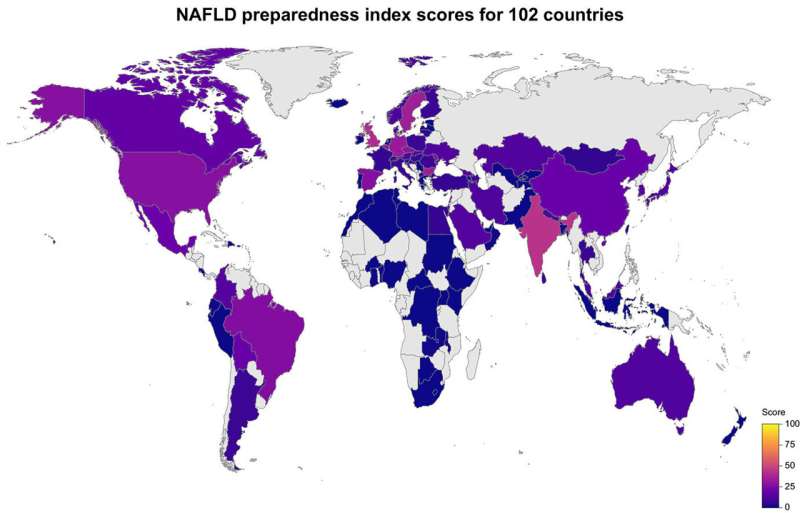
Equally concerning is that most countries do not have a national policy to manage MAFLD.
Source: Read Full Article