Lawrence Livermore National Laboratory (LLNL) researchers are studying ways to safely and rapidly remove viral threats from N95 respirators, without compromising the device’s fit and its ability to filter airborne particles, so they can be reused.
As seen during the COVID-19 pandemic, a shortage of personal protective equipment, including surgical masks and respirators, can impede efforts to help infected patients, as well as efforts to protect medical providers and first responders.
N95 respirators are protective devices that filter airborne particles. The “N95” designation means that the respirator blocks at least 95 percent of very small (0.3 micrometers or larger) test particles. They are typically used a single time in health care settings because the respirators can be contaminated when treating infected patients, thereby posing a risk to caregivers who continue wearing a contaminated device, as well as other patients treated by the provider.
According to Sal Baxamusa, who leads LLNL’s research team, they are exploring ways to deactivate the SARS-CoV-2 virus on N95 respirators using inexpensive tools that are readily available in hospitals, as well as field settings, to ensure the continued availability of this critical resource during a crisis.
“In health care settings, it is always preferable to use an N95 respirator just one time. But in emergency situations, additional options may need to be considered,” said Baxamusa.
LLNL’s team is studying deactivation techniques that rapidly remove the viral threat, without compromising the way the respirator fits on the user’s face, and without leaving toxic residue that could harm users. For example, liquid disinfectants like bleach can damage the filter, and sterilization methods that rely on ultraviolet light do not penetrate deep enough to fully decontaminate the filter. Sending masks off site to a central location with sophisticated decontamination equipment may not be practical during a crisis, when there is a limited supply of respirators.
Thermal process to deactivate virus
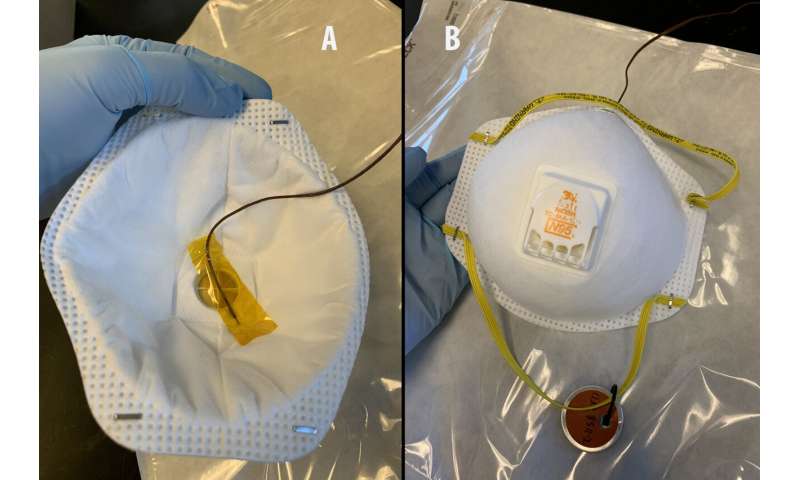
The LLNL team is testing the efficacy of using a thermal process, where heat penetrates through the outer cover of the respirator to deactivate the virus on internal parts, including the filtering element. At the same time, they are studying whether respirators retain functionality after thermal treatment.
Using a standard laboratory oven, the team conducted initial tests regarding how thermal treatment affects respirator components that play a key role in ensuring a secure fit on the user’s face, such as the metal nose clip, nose foam and neck straps. Following treatment, they tested the fit of the masks in LLNL’s respirator shop and identified thermal conditions that do not compromise the fit.
With these initial tests completed, the team is now studying deactivation efficacy. Using a mouse hepatitis virus that is related to SARS-CoV-2 but does not cause disease in humans, they are investigating whether any live virus remains on the filter of an N95 respirator after heat treatment. Following treatment, they will gently remove viral particles from the material and count the number of infectious particles that are present.
While thermal treatment does not completely decontaminate all pathogens, the research team anticipates that it can deactivate viruses.
“We are thrilled to be part of this effort to explore options for field-based reuse of respirators,” said Bob Maxwell, who leads LLNL’s Materials Science Division. “This type of solution would make it possible to safely reuse respirators during a pandemic, or any other situation where supplies are limited, and front-line health care workers need protection.”
Source: Read Full Article



