A novel urine screening test that uses a protein, keratin 17 (K17), as a cancer biomarker reveals the test detects the presence of new or recurrent cases of bladder cancer. The methodology behind the test stems from research at Stony Brook University led by Kenneth Shroyer, MD, Ph.D. A study that details the finding of the test will be published in the American Journal of Clinical Pathology.
Some 81,000 cases of bladder cancer are diagnosed in the United States each year according to the American Cancer Society. Accurate detection of bladder cancer, or urothelial carcinoma (UC), is often difficult, expensive and involves invasive testing. Going forward, this new method, based on the detection of K17 in urine specimens, could help guide treatment by improving diagnostic accuracy.
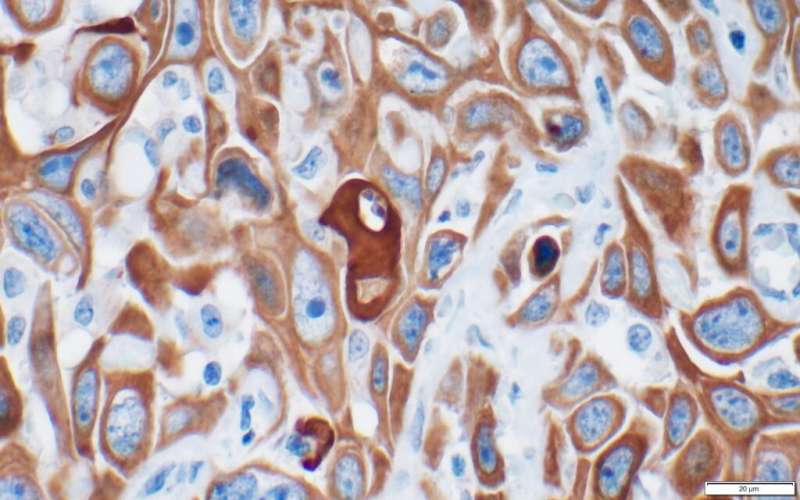
“It is important to find new biomarkers to more accurately detect UC since standard methods used in most cytology labs are based primarily on microscopic details that do not always clearly distinguish cancer from benign cells,” explains Dr. Shroyer, the Marvin Kuschner Professor and Chair of Pathology at the Renaissance School of Medicine at Stony Brook University and inventor of the K17 test.
Previously, Dr. Shroyer and his colleague, Dr. Luisa Escobar-Hoyos (an Assistant Professor at Yale), co-directed a team of Stony Brook University students and collaborators to demonstrate that K17 is a highly sensitive and specific biomarker for UC in tissue biopsy and surgical specimens. The current published study builds on these findings to show that K17 testing could also be performed as a non-invasive test on urine specimens.
Using various urine sample sets, the Stony Brook team found that the urine K17 test detected UC in 35/36 (97 percent) of cases that were confirmed by biopsy, including 100 percent of cases with high-grade UC.
From these results and other findings based on the testing, the authors conclude that K17 testing is a highly sensitive and specific diagnostic test for initial screening and for detection of recurrence across all grades of UC.
Dr. Shroyer and his colleagues believe the potential of this test as a non-invasive way to detect UC will help to transform not only diagnostic practices but earlier treatment intervention and prognosis of UC.
Source: Read Full Article



