An investigational outpatient endoscopic procedure may help eliminate the need for insulin in people with type 2 diabetes, early research suggests.
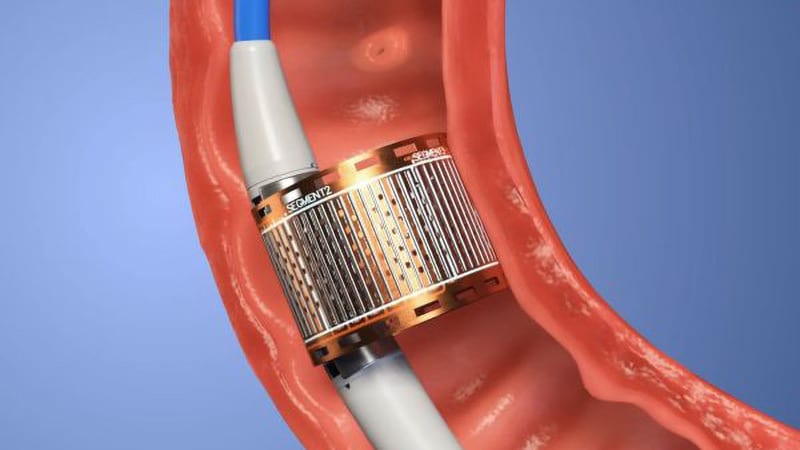
Called re-cellularization via electroporation therapy (ReCET), the technology, manufactured by Endogenex, uses a specialized catheter to deliver alternating electric pulses to the duodenum to induce cellular regeneration. This process is thought to improve insulin sensitivity, in part, by altering gut hormones and nutritional sensing, principal investigator Jacques Bergman, MD, PhD, said in a press briefing held in conjunction with Digestive Disease Week (DDW), where he will present the data on May 9.
In the first-in-human study of ReCET, 12 of 14 patients were able to come off insulin for up to a year following the procedure when combined with the use of the glucagon-like peptide-1 agonist semaglutide.
“This might be a game changer in the management of type 2 diabetes because a single outpatient endoscopic intervention was suggested to have a pretty long therapeutic effect, which is compliance-free, as opposed to drug therapy that relies on patients taking the drugs on a daily basis,” said Bergman, professor of gastrointestinal endoscopy at Amsterdam University Medical Center, Netherlands.
Moreover, he added, “this technique is disease-modifying, so it goes to the root cause of type 2 diabetes and tackles the insulin resistance, as opposed to drug therapy, which at best, is disease-controlling, and the effect is immediately gone if you stop the medication.”
ReCET is similar to another product, Fractyl’s Revita DMR, for which Bergman was involved in a randomized clinical trial. He told Medscape Medical News that the two technologies differ in that the Revita uses heat with submucosal lifting to avoid deeper heat penetration, whereas ReCET is nonthermal. He is also involved in a second randomized trial of the Revita.
Is Semaglutide Muddying the Findings?
Asked to comment about the current study with ReCET, Ali Aminian, MD, professor of surgery and director of the Bariatric and Metabolic Institute at the Cleveland Clinic, Ohio, told Medscape Medical News that the treatment effect is certainly plausible.
“The observation that hyperglycemia rapidly and substantially improves after bariatric surgery has prompted innovators to search for novel endoscopic procedures targeting the GI tract to improve diabetes and metabolic disease. Over the years, we learned that in addition to its role in digestion and absorption, the GI tract is actually a large endocrine organ which contributes to development of diabetes and metabolic disease.”
However, Aminian said that “while these preliminary findings on a very small number of patients with a very short follow-up time are interesting,” he faulted the study design for including semaglutide. “When patients are treated with a combination of therapies, it will be hard to understand the true effect of each therapy,” and particularly, “when we add a strong diabetes medication like semaglutide.”
Bergman said semaglutide was used to “boost the insulin-resistant effect of the endoscopic treatment,” and that a planned double-blind randomized trial will “show how much semaglutide actually contributed to the effect.” The ultimate goal, he noted, is to eliminate the need for all medications.
Moreover, when people with type 2 diabetes add semaglutide to insulin treatment, only about 20% typically are able to quit taking the insulin, in contrast to the 86% seen in this study, lead author Celine Busch, MBBS, a PhD candidate in gastroenterology at Amsterdam University, said in a DDW statement.
Aminian said, “I’m looking forward to better quality data…from studies with a stronger design to prove safety, efficacy, and durability of this endoscopic intervention in patients with diabetes.”
But, he also cautioned, “in the past few years, other endoscopic procedures targeting the duodenum were introduced with exciting initial findings based on a small series [with a] short-term follow-up time. However, their safety, efficacy, and durability were not proven in subsequent studies.”
All Patients Stopped Insulin, Most for a Year
The single-arm, single-center study involved 14 patients with type 2 diabetes taking basal but not pre-meal insulin. All underwent the 1-hour outpatient ReCET procedure, which involved placing a catheter into the first part of the small bowel and delivering electrical pulses to the duodenum.
Patients adhered to a calorie-controlled liquid diet for 2 weeks, after which they were initiated on semaglutide. All 14 patients were able to come off insulin for 3 months while maintaining glycemic control, and 12 were able to come off insulin for 12 months. They also experienced a 50% reduction in liver fat.
Bergman said a randomized, double-blind study using a sham procedure for controls is expected to start in about 2 months. “But for now, we are very encouraged by the potential for controlling type 2 diabetes with a single endoscopic treatment.”
Bergman has reported serving on the advisory board for Endogenex. Aminian has reported receiving research support and honorarium from Medtronic and Ethicon.
Digestive Disease Week 2023. Abstract #1272. To be presented May 9, 2023.
Miriam E. Tucker is a freelance journalist based in the Washington, DC, area. She is a regular contributor to Medscape, with other work appearing in The Washington Post, NPR’s Shots blog, and Diabetes Forecast magazine. She is on Twitter: @MiriamETucker.
For more diabetes and endocrinology news, follow us on Twitter and Facebook.
Source: Read Full Article