Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has infected millions worldwide, causing respiratory coronavirus disease 2019 (COVID-19) and a global pandemic. Rapid development and deployment of different COVID-19 vaccines and non-pharmaceutical interventions, such as hard and soft lockdowns, have been effective in curbing numbers of daily new infections, hospitalizations, and deaths globally.
However, while vaccines represent the most likely way to protect oneself from severe COVID-19 and related hospitalization, antibody responses and neutralizing activity have been shown to wane over the months following SARS-CoV-2 primary infection and after vaccination.
SARS-CoV-2 variants with mutations in the spike protein that help the virus evade host immune responses add to this problem in convalescents and vaccinees. They have become a significant obstacle to ending this pandemic.
So far, four variants – B.1.1.7 (alpha or UK variant), B.1.351 (beta, RSA), P.1 (gamma, BRA) and B.1.617.2 (delta, IND) have been termed as variants of concern (VoC) owing to their ability to spread and cause breakthrough infections even among the vaccinated.
After primary infection and in parallel with the antibody response, symptomatic COVID19 convalescents generate a robust CD4+ and CD8 + memory T cell response which targets a broader range of antigens and epitopes than that covered by antibodies. Importantly, as per studies, the breath of SARS-CoV-2-specific T cell epitopes appears to be less sensitive to mutations present in VoC. To date, the extent of protection offered by T-cells against re-infection and progression to severe COVID-19.
Researchers conducted a comprehensive, longitudinal, long-term immune study, including functional assays to assess immune fitness against antigenically different VoC. The study is currently available on the preprint server medRxiv* while awaiting peer review.
About the study
The said COVID-19 immunity study was conducted 12 months after PCR confirmed SARS-CoV-2 infection and in the complete absence of community transmission in a South Australian cohort of 43 mild COVID-19 convalescents.
An in-depth evaluation of multi-isotype antibody responses, homologous pseudotyped virus, homologous and VoC live-virus serum neutralization activity, RBD-specific B cell populations and Spike and non-Spike SARS-CoV-2 specific CD8+ and CD4+ T cell immunity against ancestral and VoC antigenic epitopes were done.
Results were compared to age- and gender-matched COVID-19 naïve, healthy individuals and to COVID-19 convalescent responses at 6 months after infection in the same cohort.
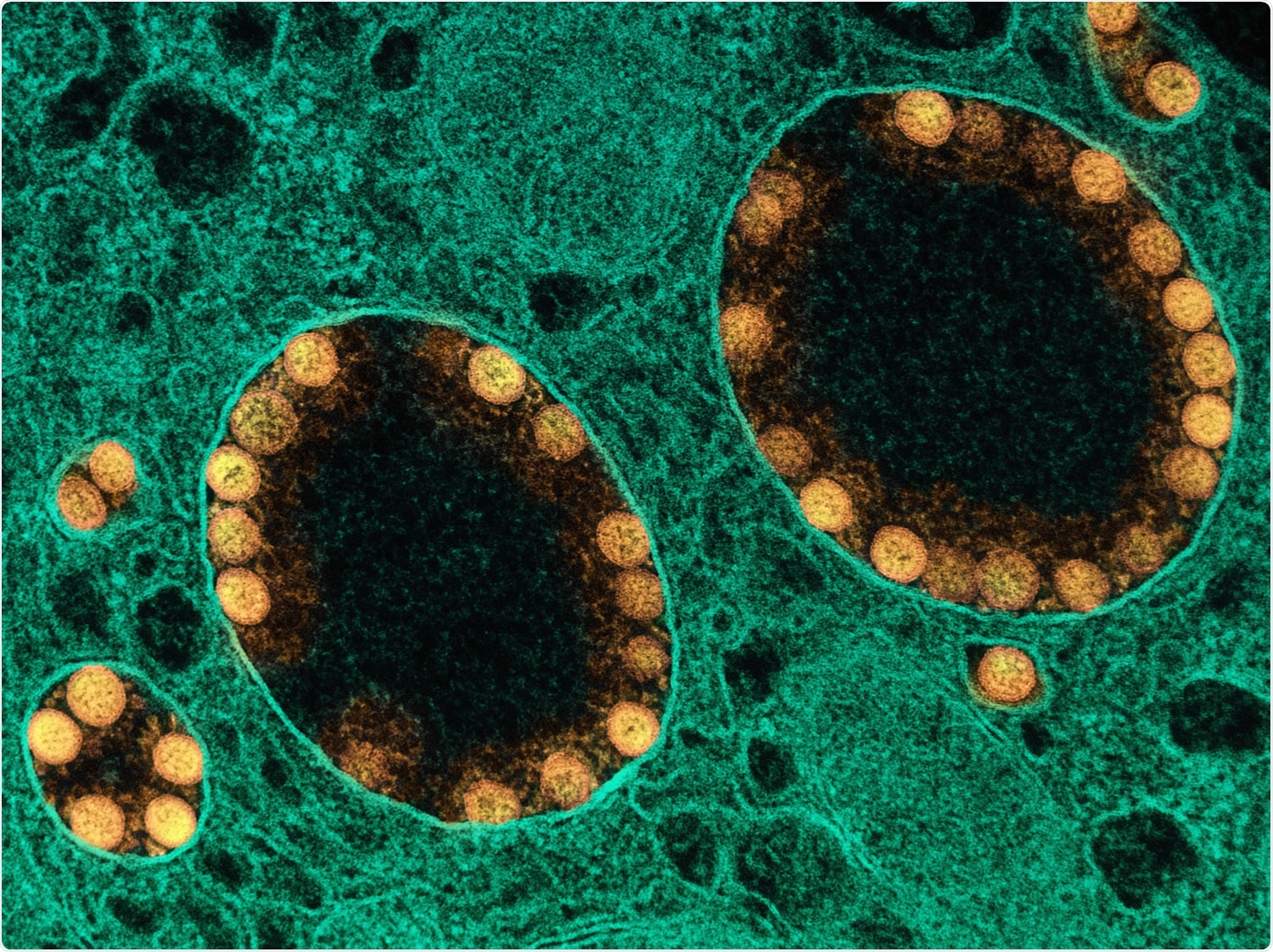
The receptor-binding domain (RBD) of SARS-CoV-2 Spike protein is the main target of neutralizing antibodies (nAb), and nAb titers decline in the months after COVID-19 infection.
.jpg)
Analyzing the longitudinal effect of humoral responses indicated that despite a high prevalence of Receptor Binding Domain (RBD)-seropositivity, existence of circulating memory B cells and homologous virus neutralization activity among COVID19 convalescents, functional humoral responses to VoC reduced significantly at 12 months post-infection.
At 12 months after mild-COVID-19, >90% of convalescents remained seropositive for RBD-IgG and 88.9% had circulating RBD-specific memory B cells. Despite this, only 51.2% of convalescents had serum neutralizing activity against homologous live-SARS-CoV-2 virus, which further reduced to 44.2% when tested against live B.1.1.7 (alpha), 4.6% against B.1.351 (beta), 11.6% against P.1 (gamma) and 16.2%, against B.1.617.2 (delta) VoC.
The spike and non-spike-specific T cells were detected in >50% of convalescents with frequency values higher for Spike antigen as compared to non-Spike antigens.
Despite the high prevalence and maintenance of Spike-specific T cells in Spike ‘high responders’ convalescents (convalescents with Spike-specific CD4+ and CD8+ T cell responses, higher than a statistically determined threshold) well above healthy control levels at 12 months, T-cell functionality, as measured by cytokine expression after stimulation with Spike epitopes corresponding to VoC was considerably reduced.
These data suggest that suboptimal Spike-specific T helper cell functional responses are more likely to occur in convalescents (infected with Wuhan-like variants) who encounter B.1.351 or B.1.617.2, rather than other VoC. This is similar to what happens with humoral antibody responses in COVID-19 convalescents and vaccinees alike.
Implications
The study reveals that, despite the durability and maintenance of serum antibodies, circulating memory B cells and T cell responses at 12 months after the original infection, COVID-19 convalescents have pronounced deficiencies in functional Spike-specific T cell responses and the ability to neutralize the current VoCs.
These results highlight the need to continue vaccination even among people with previously reported mild COVID-19 and imply the risks of re-infection with severely virulent VoCs due to a delay in vaccination.
These studies are more relevant in the context of the existing worldwide inequalities in vaccine distribution, which have kept many developing countries from Africa, Southeast and South Central Asia and Central America at vaccination rates of 20-30% (for full vaccination).
*Important notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
Reference:
- COVID-19 convalescents exhibit deficient humoral and T cell responses to variant of concern Spike antigens at 12 month post-infection Pablo Garcia-Valtanen, Christopher M. Hope, Makutiro G. Masavuli, Arthur Eng Lip Yeow, Harikrishnan Balachandran, Zelalem A. Mekonnen, Zahraa Al-Delfi, Arunasingam Abayasingam, David Agapiou, Alberto Ospina Stella, Anupriya Aggarwal, Jason Gummow, Catherine Ferguson, Stephanie O’Connor, Erin M. McCartney, David J. Lynn, Guy Maddern, Eric J Gowans, Benjamin AJ Reddi, David Shaw, Chuan Kok-Lim, Stuart G Turville, Michael R Beard, Daniela Weiskopf, Alessandro Sette, Rowena A. Bull, Simon C. Barry, Branka Grubor-Bauk medRxiv 2021.11.08.21266035; doi: https://doi.org/10.1101/2021.11.08.21266035, https://www.medrxiv.org/content/10.1101/2021.11.08.21266035v1
Posted in: Medical Research News | Disease/Infection News
Tags: Antibodies, Antibody, Antigen, B Cell, CD4, Cell, Cell Death, Coronavirus, Coronavirus Disease COVID-19, Cytokine, Frequency, Homologous, immunity, Pandemic, Protein, Pseudovirus, Receptor, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Spike Protein, Syndrome, T-Cell, Vaccine, Virus

Written by
Sreetama Dutt
Sreetama Dutt has completed her B.Tech. in Biotechnology from SRM University in Chennai, India and holds an M.Sc. in Medical Microbiology from the University of Manchester, UK. Initially decided upon building her career in laboratory-based research, medical writing and communications happened to catch her when she least expected it. Of course, nothing is a coincidence.
Source: Read Full Article



