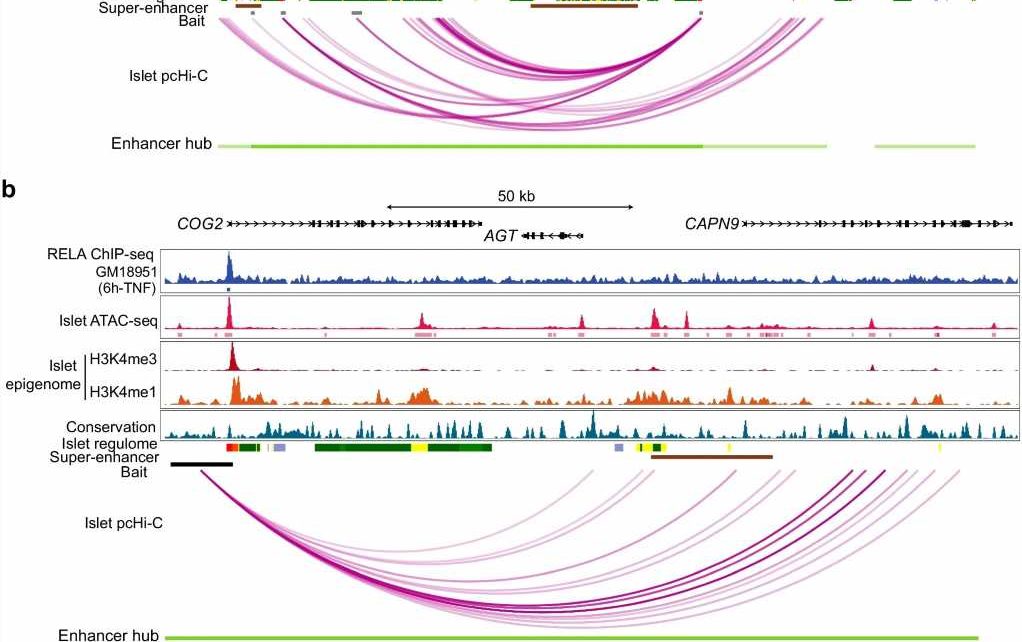
![SLC2A2 and CAPN9 locuses form part of the islet enhancer hubs linked with p65 regulation. (a, b) p65 ChIP-seq enrichment, epigenomic annotations and high-confidence pcHi-C interactions from islet samples at the two candidate loci: (a) SLC2A2 and (b) CAPN9. p65 ChIP-seq data were obtained from ENCODE. Islet pcHi-C interactions and super enhancers were obtained from Miguel-Escalada et al [22]. All browser views were generated using the WashU Epigenome Browser [53]. Only the significant pcHi-C loops within the broadcast region are shown. ChIP, chromatin immunoprecipitation. (c, d) Real-time PCR analysis of (c) Slc2a2 and (d) Capn9 in islets isolated from p65fl/fl and βp65KO mice. Statistical analysis was performed using Student’s t tests. Data are means ± SEM. *p<0.05, ***p<0.001. Credit: Diabetologia (2023). DOI: 10.1007/s00125-023-05931-6 Gene provides clues for preventing common diabetes side effect of corticosteroid treatment](https://scx1.b-cdn.net/csz/news/800a/2023/gene-provides-clues-fo.jpg)
A study led by researchers at the Garvan Institute of Medical Research shows for the first time how a gene called RELA, known to regulate inflammation, also plays an essential role in maintaining normal blood-sugar levels.
The findings, published in Diabetologia, have implications for the prevention of steroid-induced diabetes, a temporary form of diabetes that affects up to half of hospital patients treated with high-dose steroids.
“Our discovery sheds new light on a complex network of factors governing glucose metabolism and how it can go awry in diabetes,” says Professor Shane Grey, senior author of the paper and Head of the Transplant Immunology Lab at Garvan. “Steroids are known help prevent inflammation by targeting RELA. Our finding that RELA also coordinates the expression of genes in the pancreas that are essential for glucose control and preventing diabetes therefore has major implications for understanding and preventing steroid-induced diabetes, which could be achieved using treatment strategies that prevent inflammation without targeting RELA.”
Double duty: RELA gene controls inflammation and insulin secretion
Inflammation is a key target for therapy. Though at the center of the body’s defense mechanisms, inflammation can cause harm and autoimmune disease when it goes unchecked.
To better understand the mechanisms behind inflammation and how they may be better targeted, the Garvan-led researchers studied different genes that control inflammation in the body, using mouse models. They found a surprising effect—removing a gene called RELA, which helps regulate the expression of proteins involved in inflammation, led to abnormally high blood-sugar levels.
“When we removed RELA from the system, we found that our models became pre-diabetic. We found this was due to impaired insulin secretion in the beta cells of the pancreas,” says lead author Dr. Nathan Zammit, Visiting Scientist at Garvan.
The researchers next investigated the cells lacking RELA using next-generation DNA analysis techniques.
“Interestingly, we found that the protein RELA produces directly switches on a genetic program required for cells in the pancreas to produce insulin. This indicated that even though inflammation and diabetes are known to be linked, RELA regulates blood sugar and inflammation completely independently. Our findings suggest that RELA plays an essential role in keeping blood-sugar levels normal, even when there is no inflammation,” says Dr. Zammit.
The team’s findings have implications for developing more tailored therapies for patients that require corticosteroid treatment, a class of drugs commonly used to reduce inflammation in the body in conditions such as arthritis or asthma.
Within weeks of starting or increasing a dose of corticosteroid medications, patients can develop steroid-induced diabetes. Until now, the mechanism of this link between inflammation and diabetes was not well understood.
“While our research has uncovered a new fundamental facet of how our body maintains normal blood glucose levels, the findings could also help improve clinical management of patients who require long-term or high-dosage corticosteroid treatment,” says Professor Grey.
“By understanding how insulin-producing cells and systems in the pancreas are regulated by RELA, it may be possible to balance the inhibition of inflammation without disrupting the function of insulin-producing cells. This could lead to the development of medications that reduce inflammation without bringing on steroid-induced diabetes as a side effect.”
More information:
Nathan W. Zammit et al, RELA governs a network of islet-specific metabolic genes necessary for beta cell function, Diabetologia (2023). DOI: 10.1007/s00125-023-05931-6
Journal information:
Diabetologia
Source: Read Full Article