New research has laid the groundwork for a long-lasting eye drop to treat corneal neovascularisation (CoNV), a condition which affects more than a million people globally each year.
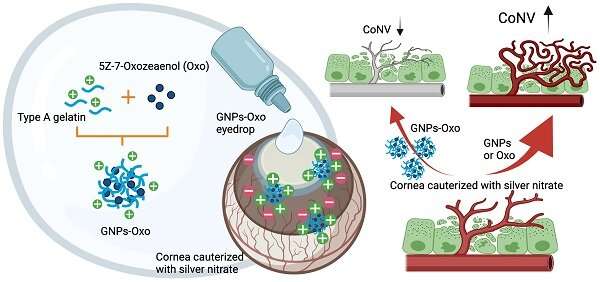
A pre-clinical study, led by Associate Professor Rick Guei-Sheung Liu and Dr. Sloan Wang, published in the Theranostics journal, tests the use of nanomedicine to deliver drugs used to treat damaged corneas.
Dr. Liu says the technique has enormous potential—and could be used by other scientists trying to deliver drugs to treat other eye conditions.
He hopes the current research will lead to new treatments for corneal neovascularisation that are more effective than current therapies and only need to be administered once a day.
Corneal neovascularisation
The cornea is the clear window at the front of the eye. It allows light to enter the eye and does most of the focusing for the eye.
The cornea must be clear to allow light to pass into the eye. It must also have a regular curve to properly focus the light.
But trauma, toxic chemical injuries and infections like chronic belpharoconjunctivitis or keratitis can cause new blood vessels to form and extend deep into the cornea, causing it to cloud and interfere with vision.
In the advanced stages, the condition can lead to significant vision loss and also cause corneal transplants to fail.
Nanoparticle promise
Associate Professor Liu, who is the head of Genetic Engineering Research at CERA, completed the current study when he was at the University of Tasmania in collaboration with the Taipei Medical University.
The team used nanoparticles, sub-microscopic particles, to develop a gelatin-based eye drop system that could deliver effective and long-lasting treatment to the corneal surface.
If developed as a treatment in clinical trials, the nanoparticle eye drop could potentially prove more effective at preventing vision loss than traditional eye drops.
The eye drops would be less invasive than other types of treatments, such as eye injections or surgery, which may have limited benefits and can cause side effects.
Associate Professor Liu says that by using nanoparticle formulation, the new drops would be ‘stickier,” more effective and last longer than traditional eye drops.
“You constantly need to use eye drops, three or four times a day, even more frequently, to stop the deterioration of the cornea,” he says.
“We enabled a nanoparticle to carry a drug as an eye drop, so that the particle can stick to the cornea and then slowly release the drug, resulting in better treatment outcomes for corneal disease.
“We demonstrated that with just one drop a day you can minimize this severe corneal deterioration.”
Improving corneal transplants
Associate Professor Liu says corneal transplant outcomes could also be improved by halting further tissue damage and preventing excessive blood vessel growth in the lead-up to surgery.
Following a transplant, the new cornea needs to ‘take’ after being attached to existing tissue. Associate Professor Liu says the more damaged the cornea and surrounds, the poorer the outcome.
“The success of a corneal transplant depends upon the health of the cornea before the operation,” he says.
“If your tissue remains in good condition, when you stitch the new cornea to the old tissue it will heal pretty well. We need to stop any potential deterioration of the cornea before an implant is required, otherwise it could fail.”
Looking to the future
Associate Professor Liu says the new technology could greatly improve outcomes for people with serious corneal problems, and lead to similar eye drops for other eye diseases.
It could potentially replace eye injections and in some cases help to avoid invasive surgery.
“You can modify the formulation to treat retinal disease,” says Associate Professor Liu.
“The nanoparticle can also help drugs reach deep into the retinal tissue from the eye surface. We can then use the eye drop system to transport drugs to treat retinal conditions there, without need for an invasive eye injection.
“This is a simple but effective way to get our medicines where we want them to go without probing or poking around the eye.”
Source: Read Full Article



