A recent review paper published in the MDPI's journal Viruses highlights how available vaccines may be effective in protecting individuals against severe forms of coronavirus disease 2019 (COVID-19), but the protection against infection with the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and its transmission to others may be reduced – with consequences for community protection and herd immunity.
.jpg)
Following the infection with SARS-CoV-2, a causative agent of the current COVID-19 pandemic, there is an activation of both innate and adaptive immune systems in our body. Thus, in many ways, the disease severity depends on how we respond to the infection.
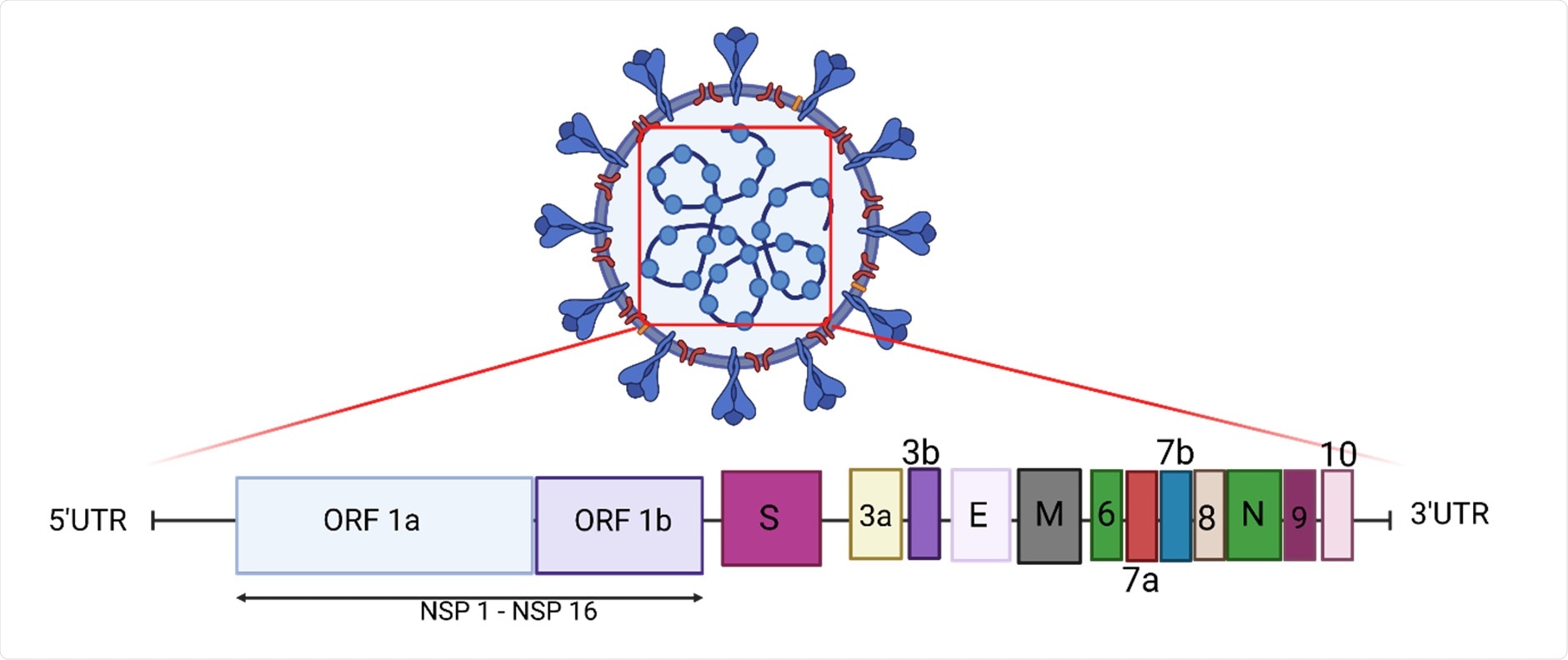
Neutralizing antibodies that are generated are highly specific for viral epitopes predominantly found in the SARS-CoV-2 spike glycoprotein, but T cells are also recruited in order to secrete antiviral cytokines and kill infected cells.
If the early immune response of the host is unable to control and clear the virus, the disease marches toward a secondary phase characterized by an uncontrolled host inflammatory response, which is responsible for known severe manifestations and may finally result in organ damage.
This is why vaccines were the real game-changer in this pandemic. Even though we are only a little more than 18 months into the pandemic, four vaccines are already widely used around the world: Pfizer/BioNtech's BNT162b2, Moderna's mRNA-1273, Janssen's Ad26.COV2S and AstraZeneca's ChAdOx1.
A swift rise of viral variants
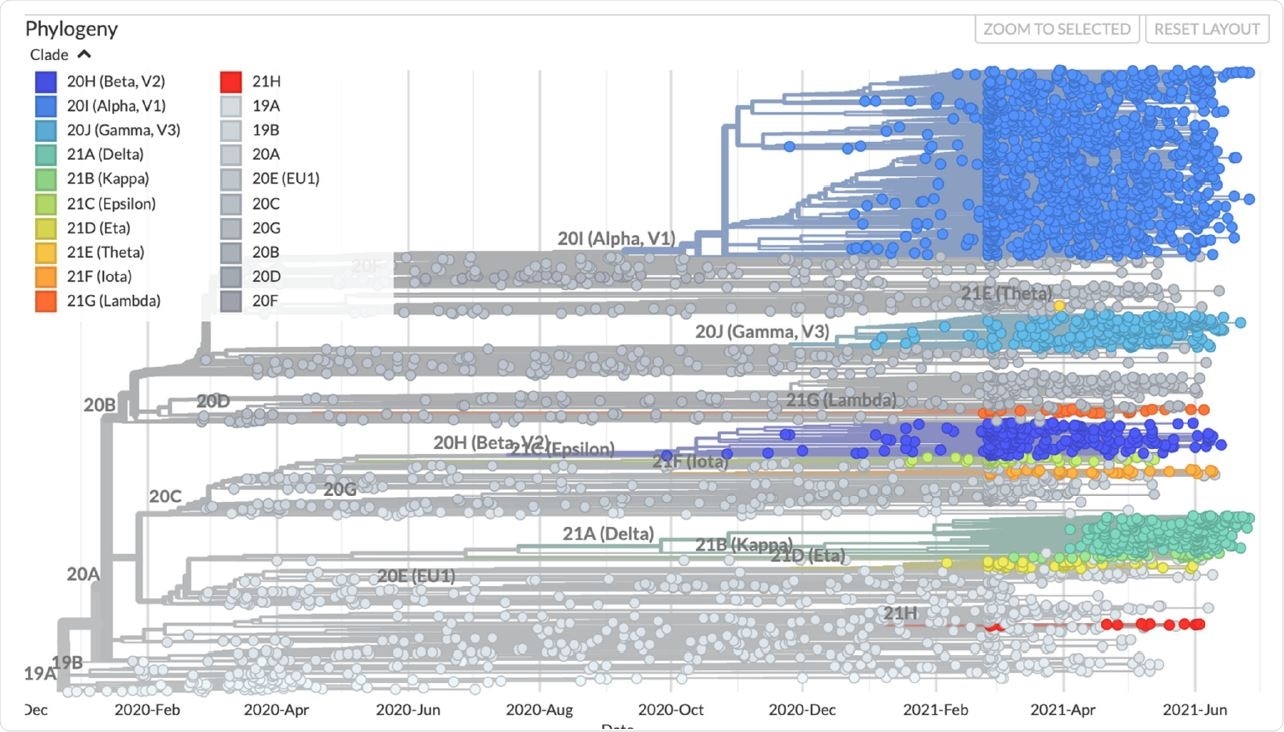
However, towards the end of 2020, there was already an emergence of several different SARS-CoV-2 variants of concern (as a result of mutational changes in the viral genome) that showed increased transmissibility and possible evasion of immune responses generated from prior SARS-CoV-2 infection.
Of note, variants of concern are those strains of SARS-CoV-2 that have higher transmissibility rates, more severe clinical presentations, lower response to treatment, or inadequate diagnostic yields with the use of established procedures and tests.
Likewise, these viral variants are also a threat to the efficacy of vaccines. As a result of the presence of mutations in spike glycoprotein (especially in neutralizing antibody epitopes), laboratory experiments have revealed a drop in the ability of post-vaccination serum samples to neutralize variants of concern.
The possibility of reinfection
Even though variants of concern carry mutations that elude complete neutralization by the antibodies, and there are several reports of reinfections, it is still unclear whether the risk of reinfection is actually increased. Theoretically, the risk is there if spike glycoprotein changes, primarily due to its role in cell entry and because it is targeted by protective antibodies.
Some studies show that this may indeed be the case, but it depends on the variant in question. A study from the United Kingdom proved reinfection in 0.7% of tested individuals, but this did not correlate with the proportion of infections in those regions caused by the alpha variant – indicating a minor effect of this variant on the risk of reinfection.
On the other hand, a longitudinal serological study of unvaccinated repeat blood donors from Manaus in Brazil showed that, in the midst of the emergence of the gamma variant, a total of 16.9% of presumed infections had serological proof of prior infection with SARS-CoV-2.
Vaccines and variants of concern
While the effectiveness of vaccines at protecting against symptomatic infection with variants of concern may be decreased, everything points to the conclusion that they remain somewhat effective in preventing severe forms of COVID-19, hospitalization and/or death. It is also known that cellular immune responses remain largely preserved.
Nevertheless, at the moment, it is unclear whether variant-specific boosters will be necessary going forward. Such booster vaccines could either use the spike glycoprotein from the original SARS-CoV-2 Wuhan strain or the one derived from a variant of concern. Data from Israel demonstrate that a third shot during the widespread circulation of delta variant can definitely provide short-term protection against confirmed infection and severe disease.
However, it remains to be seen whether the spike protein will be able to mutate further to evade immune responses while at the same time preserving high levels of infectivity. Along with the kinetics of immune responses, this will ultimately determine whether updated vaccines or boosters will be required and at what frequency
- Torbati, E., Krause, K.L. & Ussher, J.E. (2021). The Immune Response to SARS-CoV-2 and Variants of Concern. Viruses. https://doi.org/10.3390/v13101911, https://www.mdpi.com/1999-4915/13/10/1911
Posted in: Medical Research News | Disease/Infection News
Tags: Antibodies, Antibody, Blood, Cell, Coronavirus, Coronavirus Disease COVID-19, Cytokines, Diagnostic, Efficacy, Frequency, Genes, Genome, Genomic, Glycoprotein, Immune Response, immunity, Laboratory, Membrane, Pandemic, Protein, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Spike Protein, Syndrome, Virus

Written by
Dr. Tomislav Meštrović
Dr. Tomislav Meštrović is a medical doctor (MD) with a Ph.D. in biomedical and health sciences, specialist in the field of clinical microbiology, and an Assistant Professor at Croatia's youngest university – University North. In addition to his interest in clinical, research and lecturing activities, his immense passion for medical writing and scientific communication goes back to his student days. He enjoys contributing back to the community. In his spare time, Tomislav is a movie buff and an avid traveler.
Source: Read Full Article



