Because of the opioid crisis, physicians are less likely to administer opioids to help manage patients’ pain, even in the operating room.
A recent analysis in JAMA Surgery conducted by investigators at Massachusetts General Hospital (MGH) indicates that overly restricting use of opioids during surgery may be doing more harm than good.
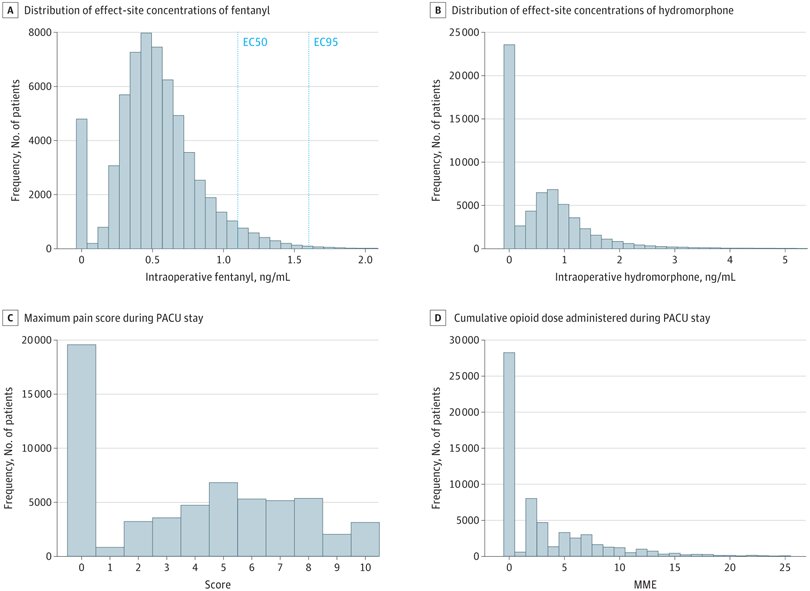
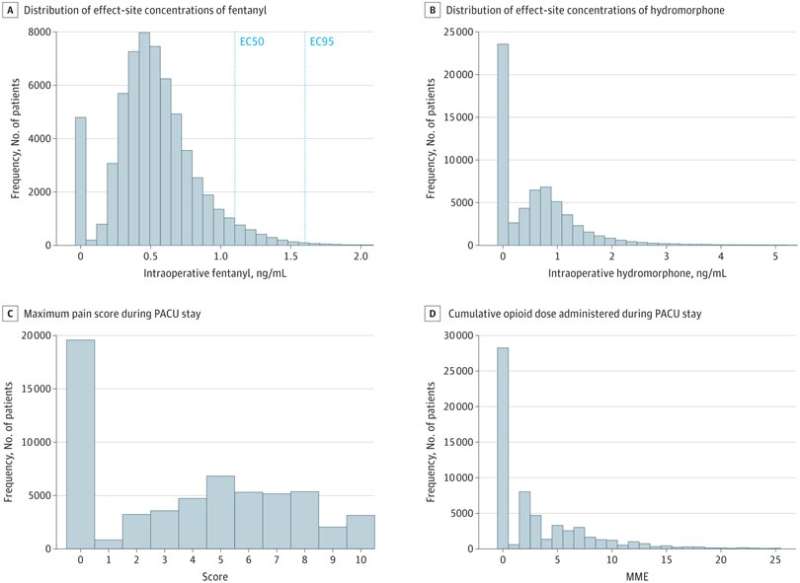
For the study, researchers analyzed information on 61,249 adults who had surgery at MGH from 2016–2020. Patients who were administered more of the opioids fentanyl and hydromorphone during surgery were less likely to experience pain and required fewer opioids in the hospital after waking up from anesthesia.
Also, patients exposed to higher amounts of fentanyl were less likely to experience uncontrolled pain or to experience new chronic pain diagnosed within 3 months of surgery; were less likely to be prescribed opioids at 30, 90, and 180 days after surgery; and were less likely to develop new persistent opioid use, all without an increase in adverse effects.
“Our analysis adjusts for many factors that might influence the decision to give opioids intraoperatively, and accounts for the known properties of the drugs. Because of this we feel confident that the opioid exposure during surgery is driving this result,” says co-first author Ran Liu, Ph.D., a research fellow in the Department of Anesthesia, Critical Care, and Pain Medicine at MGH.
The findings point to the importance of ensuring that patients don’t emerge from general anesthesia in pain, not only for their short-term well-being but also to safeguard against persistent pain and the need for prolonged opioid use.
“The opioid crisis is a major motivator for mitigating the risks of opioid usage,” says co-first author Laura A. Santa Cruz Mercado, MD, anesthesiology resident in the Department of Anesthesia, Critical Care, and Pain Medicine at Beth Israel Deaconess Medical Center and former research fellow in the Department of Anesthesia, Critical Care, and Pain Medicine at MGH. “But appropriate opioid administration in the operating room may reduce total opioid usage after surgery.”
Co–senior author Patrick L. Purdon, Ph.D., the Nathaniel M. Sims Endowed Chair in Anesthesia Innovation and Bioengineering at MGH and an associate professor of Anesthesia at Harvard Medical School, notes that additional research is needed to provide more clear guidance to surgical teams.
“We need to develop new technologies to help anesthesiologists titrate and optimize opioid administration in the operating room in a personalized way,” he says. “But this data gives us evidence that such efforts could have significant long-term benefits.
Laura A. Santa Cruz Mercado and Ran Liu were co–first authors on this paper. Edward A. Bittner and Patrick L. Purdon were co–senior authors. Additional co-authors include Kishore M. Bharadwaj, Jasmine J. Johnson, Rodrigo Gutierrez, Proloy Das, Gustavo Balanza, Hao Deng, Akriti Pandit, Tom A.D. Stone, Teresa Macdonald, Caroline Horgan, Si Long (Jenny Tou), and Timothy T. Houle.
More information:
Laura A. Santa Cruz Mercado et al, Association of Intraoperative Opioid Administration With Postoperative Pain and Opioid Use, JAMA Surgery (2023). DOI: 10.1001/jamasurg.2023.2009
Journal information:
JAMA Surgery
Source: Read Full Article