A COVID-19 treatment using monoclonal antibodies is one step closer thanks to the efforts of Australian researchers.
Scientists found antibodies that blocked the SARS-CoV-2 virus from entering cells in preclinical models.
The discovery paves the way for clinical trials of monoclonal antibody treatments for the prevention of severe COVID-19 infection.
Published in the journal Cell Reports, the research is part of a consortium-led effort, bringing together the expertise of Australian academic and industry leaders in infectious diseases and antibody therapeutics at WEHI, the Doherty Institute, the Burnet Institute, the Kirby Institute, CSL, Affinity Bio and CSIRO.
Antibody cocktail blocks SARS-CoV-2 from entering cells
Monoclonal antibodies have emerged as powerful therapeutics for a variety of human diseases, representing seven of the top ten best-selling drugs globally.
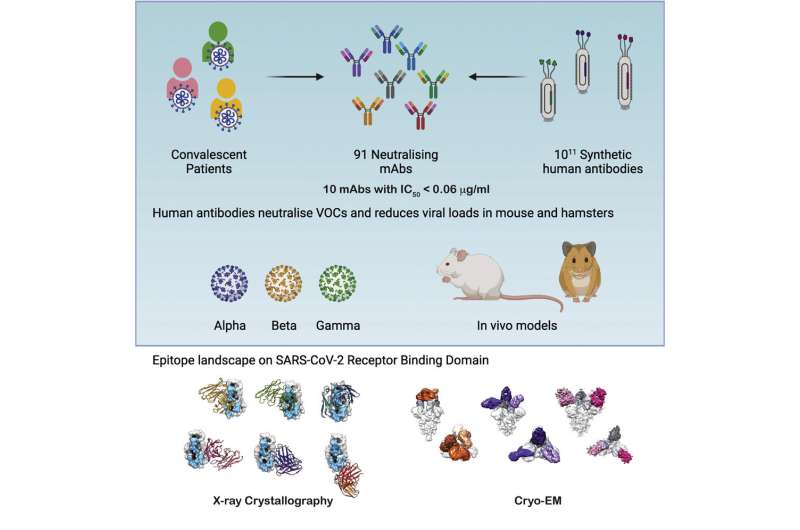
Antibodies from recovered COVID-19 patients and CSL’s proprietary antibody library were used to screen for antibodies that were effective against the SARS-CoV-2 virus. The leading two monoclonal antibodies were then combined into an “antibody cocktail.”
WEHI Associate Professor Wai-Hong Tham, who co-led the research, said the consortium had screened hundreds of potential antibodies, identifying the top 12 that were the most potent in blocking virus entry.
“By combining the leading antibodies into an antibody cocktail, we were able to test its effectiveness at blocking SARS-CoV-2 from entering cells and reducing viral loads in preclinical models,” she said.
“This antibody cocktail effectively blocked virus entry in these tests and reduced the severity of disease in preclinical models, enabling the infection to be overcome.”
“Our research indicates these monoclonal antibodies are leading candidates to be developed into a treatment for COVID-19.”
Protecting the most vulnerable
Associate Professor Tham said monoclonal antibody treatments could be used to form a “protective ring” around the most vulnerable people during an outbreak or in cases of infection in returned travelers.
“Unlike vaccines, which take several weeks to generate antibodies, antibody-based therapies would provide immediate protection against the virus,” she said.
“In the future, we may be able to use these therapies in people who are immunocompromised or unable to mount a robust immune response to a vaccine. If used early on, these treatments could prevent hospitalisations and serious complications from COVID-19.”
Jobs boost for manufacturing and industry
Doherty Institute laboratory head Professor Stephen Kent, who is an infectious diseases clinician and co-led the research, said the consortium was now working to progress the research to clinical trials in Australia.
“We recently received funding from the Medical Research Future Fund to take this promising research forward into clinical trials for COVID-19,” he said.
“Melbourne’s biomedical precinct has enormous expertise and capability. To be able to deliver a treatment for patients that was researched, designed, manufactured and trialed here in Australia would be an incredible achievement.”
“Our research shows that these monoclonal antibody therapies will be effective against global variants and could future-proof Australia against emerging coronavirus pandemics.”
The development of monoclonal antibody therapies in Australia would also provide a boost to local jobs in manufacturing, academia, biotechnology, and clinical services and strengthen Australia’s reputation as a destination for medical research innovation.
Research assisted by people who have recovered from COVID-19
COVID-19 recovered patient and nursing science student Georgie Johns, who provided blood samples for the study, said she was happy to be able to contribute to the growing body of scientific knowledge of COVID-19 in Australia.
“I contracted COVID-19 early on in the pandemic when not much was known about the virus and I really wanted to do whatever I could to help advance our knowledge about the virus in Australia,” she said.
“It is good to know these treatments might be used to help people working on the frontline in healthcare or to protect the most vulnerable people in our community, for whom vaccines might be less effective.”
Source: Read Full Article



