New insights explaining why some children have a longer remission than others after having cutting-edge CAR T-cell therapy for leukemia have been revealed by researchers at UCL, Great Ormond Street Hospital, and the Wellcome Sanger Institute.
The collaborative research project, published today in Nature Medicine, combines expertise in novel immune therapy design and state-of-the-art computational analysis to identify a genetic signature of CAR T-cells that will be the most effective in the long term.
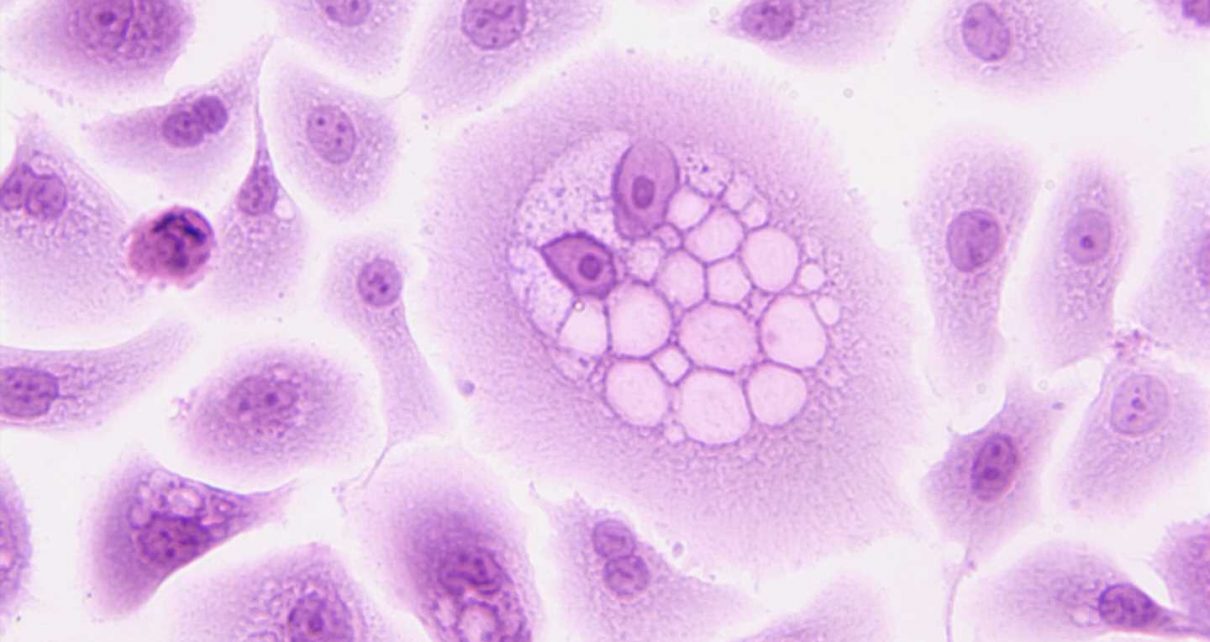
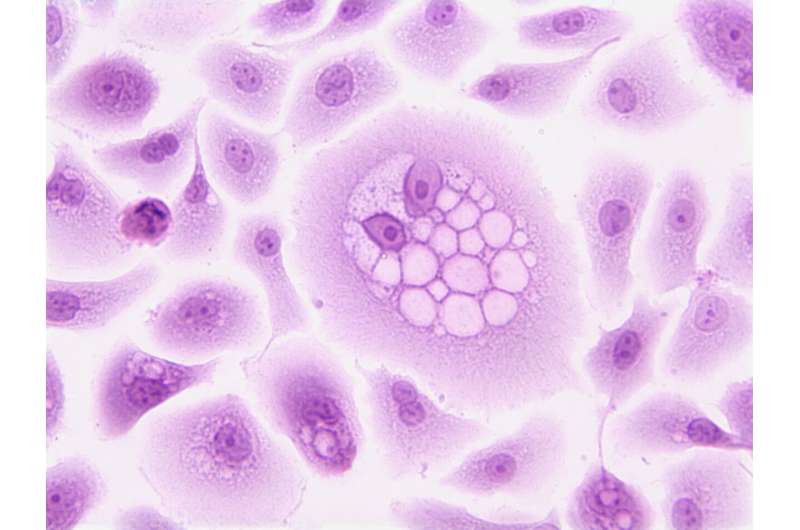
In recent years, CAR T-cells—genetically engineered T-cells (a type of immune cell) designed to target leukemia—have become an established treatment option for children with a relapsed or incurable rare form leukemia (B-cell acute lymphoblastic or B ALL).
One of the key factors that determines whether the treatment will lead to a long-lasting remission of the leukemia—allowing children to live cancer free—is how long the CAR T-cells last in the body. Until now, little has been known about what makes these cells last in the body and, therefore, whether the treatment is likely to work long-term without further therapy.
A collaborative research team from across Great Ormond Street Hospital (GOSH), the Wellcome Sanger Institute and the UCL Great Ormond Street Institute of Child Health (UCL GOS ICH) worked with families for years after their CAR T-cell treatment (called AUTO1,) as part of the CARPALL study, to begin to build a picture of why some CAR T-cells stay in the body long-term.
This work provides the first stepping-stone in understanding why some CAR T-cells persist. The team aims to build on the signature discovered in this project to identify key markers in cell populations and ultimately understand if there is a way to spot, or even create CAR T-cells that will persist long-term before treatment begins.
Dr. Nathaniel Anderson, lead author and Marie Sklodowska-Curie Fellow at the Wellcome Sanger Institute, said, “Through cutting-edge single cell genomics, we have, for the first time, been able to crack the code of persistence in CAR T-cells in children with great clarity.”
“We hope that our research will provide the first clue as to why some CAR T-cells last for a long time—which we know is vital for keeping children cancer-free after treatment. Ultimately, this work will help us to continue to improve this already life-changing treatment.”
The hope is that this knowledge will eventually enable clinical teams delivering CAR T-cell therapies to better understand which patients will best respond to treatments and enable manufacturers to optimize their methods to support persistence—leading to better outcomes for patients.
Dr. Sara Ghorashian, co-senior author, Consultant in Pediatric Hematology at GOSH and Honorary Senior Clinical Lecturer at the UCL GOS ICH, said, “This data for the first time shows us the characteristics of long-lasting CAR T-cells which are responsible not just for curing children with ALL in our study but also seen in adults treated with a different CAR T-cell product for a different type of leukemia. As such, this provides us with confidence that the signature may unlock mechanisms of CAR T-cell persistence more generally and allow us to develop better treatments.”
“We are indebted to all of the children and families who make research like ours possible—it is only through their dedication that we are able to build our understanding of these new therapies and build better treatments for children across the world.”
Studying CAR T-cells in depth
The team were able to study cells from 10 children who were enrolled in a pioneering clinical trial (CARPALL trial), for up to five years after their original CAR T-cell treatment. This has provided them with a new understanding as to why some of these CAR T-cells stay around in a patient’s bloodstream, and why others vanish early—which can in some cases allow the cancer to return.
Using techniques that analyze individual cells at a genetic level to understand what they do, the scientists were able to identify a unique “signature” in long-lasting CAR T-cells. The signature suggested that long-lasting CAR T-cells in the blood transform into a different state that enables them to continue policing the patient’s body for cancer cells.
Vitally, this signature was seen across cells and patients as well as in adults treated with a different CAR T-cell product for a different type of leukemia. But it was not identified in other types of immune cells. This suggested that the signature the authors identified may not only be a marker of these long-lasting cells but could actually be what makes them persist in the body and allows for a longer remission in children.
As part of the study, the researchers identified the key genes in CAR T-cells that appeared to enable them to persist in the body for a long time. Importantly these genes will provide a starting point for future studies to identify markers of persistence in CAR T-cell products as they are made and ultimately improve their effectiveness.
Dr. Sam Behjati, co-senior author, Group Lead and Wellcome Senior Research Fellow at the Wellcome Sanger Institute and Honorary Consultant Pediatric Oncologist at Addenbrooke’s Hospital, Cambridge, said, “This study is a fantastic step forward in our understanding of CAR T-cell persistence and illustrates the power of collaborative science and combining pioneering clinical research with cutting-edge genomic science. It is crucial that we continue to develop and build on these new treatments to help more children with leukemia across the world.”
The dedication of research families
Studies such as this are only possible because of the dedication of the children and families who take part in research. For scientists to investigate the long-term persistence of cells, children had to continue to donate cells to the study for up to five years after their initial treatment.
Austin was diagnosed with B ALL at the age of two, by the age of eight he’d been through three relapses and extensive treatment including two bone marrow transplants. By the time of his fourth relapse, he had exhausted all conventional therapy options. In October 2016, Austin received an infusion of CAR T-cells as part of the CARPALL clinical trial.
Over six years later and Austin, now 14, is still cancer free, with long-lasting CAR T-cells detectable in his blood. He is just one of 10 children who have been donating samples to this study since their infusions. His dad Scott said: “It’s not an exaggeration to say that if it wasn’t for research Austin wouldn’t be alive. The research teams at GOSH gave us so much, we wanted to give something back. Taking part in this study not only gives us that opportunity but we also hope that Austin’s data will help other families like ours in the future.”
“We actually love coming back to GOSH to see the team and keep them a part of our lives. I feel so proud that Austin has been a part of this research journey.”
This continued commitment to studies is helping researchers to better understand new, cutting-edge therapies and improve them for future families.
Dr. Henry Stennett, Research Information Manager at Cancer Research UK, who part-funded the study, said, “We know that immunotherapies such as CAR T-cell therapy have seen some great success over the years, but they don’t work in all patients, and we need to continue to work to figure out why. Studies like this one are vital for bringing us closer to making immunotherapies more effective for more cancer patients.”
More information:
Nathaniel Anderson et al, Transcriptional signatures associated with persisting CD19 CAR-T cells in children with leukemia, Nature Medicine (2023). www.nature.com/articles/s41591-023-02415-3
Journal information:
Nature Medicine
Source: Read Full Article