A new study led by Hans-Martin Jäck of the Friedrich-Alexander University Erlangen-Nuremberg in Germany engineered clusters of neutralizing monoclonal antibodies using a transgenic mouse model. A unique characteristic for the antibodies was the different ways it bound to the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and the overall reduction in the viral spread for human ACE2.
The antibodies have the potential to work against some coronavirus variants of concern. The researchers also suggest neutralizing monoclonal antibodies could be hypothetically useful for COVID-19 therapies.
The team writes:
"We report two clusters of potent non-competing SARS-CoV-2 neutralizing antibodies providing potential candidates for therapy and prophylaxis of COVID-19. The study further supports the use of transgenic animals with human immunoglobulin gene repertoires in pandemic preparedness initiatives."
The study, "A pair of non-competing neutralizing human monoclonal antibodies protecting from disease in a SARS-CoV-2 infection model", is available as a preprint on the bioRxiv* server, while the article undergoes peer review.
.jpg)
Immunization schedule for antibody production
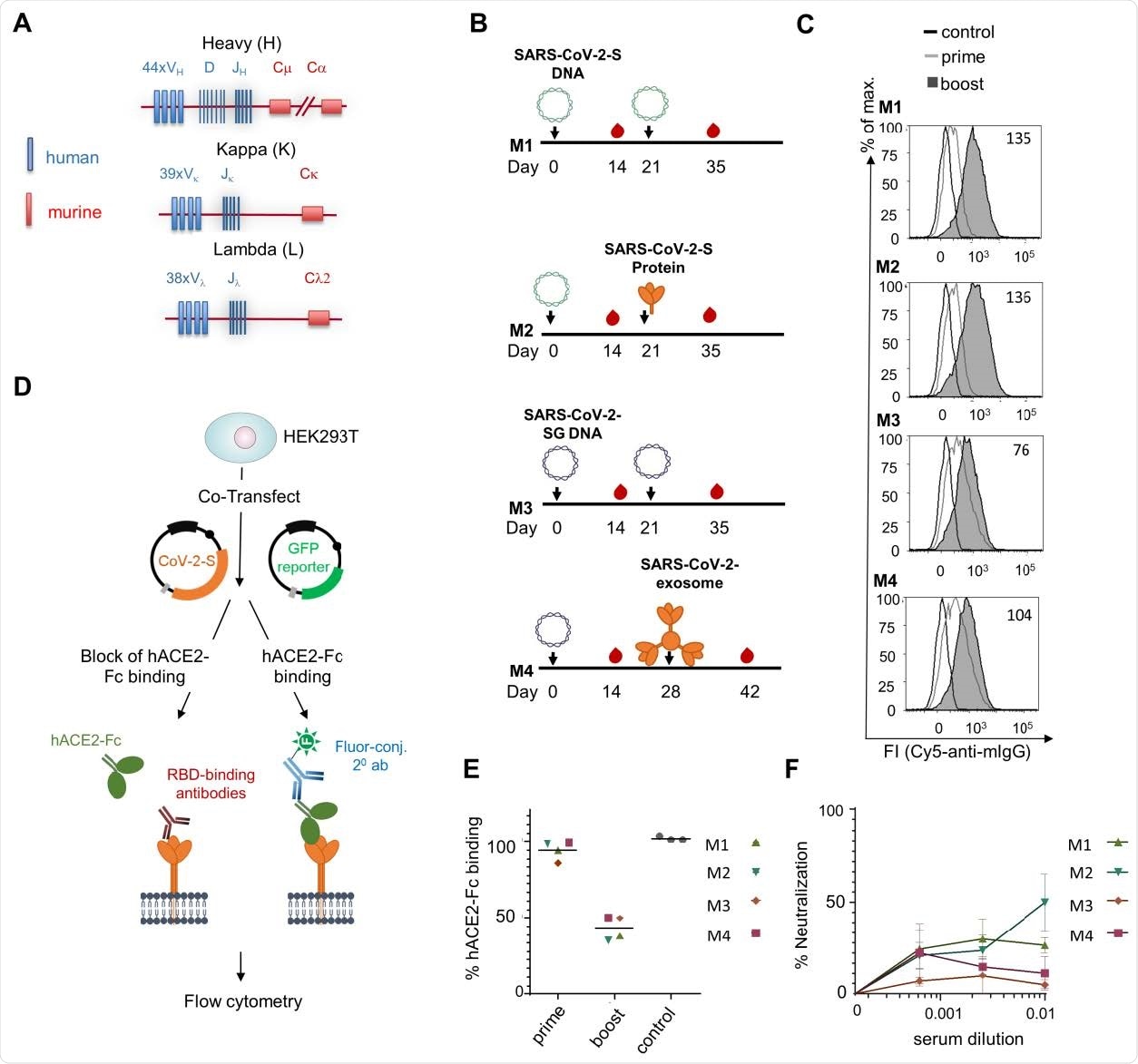
The research team used the transgenic TRIANNI mouse model to create antibodies targeting the spike protein's receptor binding domain or N-terminal domain. They chose this model because of their ability to develop antibodies with a human Ig variable region and murine constant regions.
In February 2020, the research team immunized two groups of mice intramuscularly with either the SARS-CoV-2-S DNA or the SARS-CoV-2-SG-DNA. The mice were given a booster three weeks later. The mice that received SARS-CoV-2-S DNA received either the SARS-CoV-2-S DNA or the SARS-CoV-2-S protein adjuvanted with MPLA liposomes. Meanwhile, the SARS-CoV-2-SG DNA administered SARS-CoV-2-SG at week 3 or SARS-CoV-2 exosomes at week 4.
Detection and characterization of antibodies
Antibodies specific to SARS-CoV-2 were detected after the first dose, with levels further enhancing after the second dose. In total, the TRIANNI mice produced 29 hybridoma antibodies that targeted the spike protein on the cell surface of transfected HEK293T cells. Of the 29, nine neutralized SARS-CoV-2 infection at IC50 values in the subnanomolar range.
Two weeks after the immunization regimen, the researchers tested the monoclonal antibodies produced from mice by exposing them to cells transfected with SARS-CoV-2-S DNA.
The binding properties differed across monoclonal antibodies. Some bound to the receptor-binding domain and competed for ACE2 binding, others bound to the S1 subunit only, others bound to the ectodomain of the spike protein stabilized in a trimeric form and the N-terminal domain, and others showed binding to the S2 subunit only.
When testing mice serum, they found antibodies produced direct competition to the SARS-CoV-2-S protein showed reduced viral binding two weeks after the booster shot.
Researchers produced monoclonal TRES antibodies, and with a DNA prime protein boost immunization regimen, they observed mutations in the VH and VL region. The researchers suggest this means binding affinity for the antibodies can improve against SARS-CoV-2 or potentially other viruses that cause disease such as HIV.
"Transgenic animal models supporting affinity maturation of antibodies with human variable regions should be an essential part of future pandemic preparedness efforts and be explored in structure-guided vaccine antigen design against SARS-CoV-2."
The research team also tested the neutralizing power of the monoclonal antibodies on two variants of concern. One cluster of antibodies showed potential against the B.1.351 variant, but another cluster of antibodies was ineffective against both the B.1.1.7 and B.1.351 variants of concern.
While the transgenic models produced potent neutralizing antibodies, a major downfall with this method is the long time to produce them. The complete development of human antibodies took approximately 19 weeks. However, the researchers note there is potential to shorten the immunization schedule and, therefore, reduce development time by several weeks.
*Important Notice
bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- A pair of non-competing neutralizing human monoclonal antibodies protecting from disease in a SARS-CoV-2 infection model, Antonia Sophia Peter, Edith Roth, Sebastian R. Schulz, Kirsten Fraedrich, Tobit Steinmetz, Dominik Damm, Manuela Hauke, Elie Richel, Sandra Mueller-Schmucker, Katharina Habenicht, Valentina Eberlein, Leila Issmail, Nadja Uhlig, Simon Dolles, Eva Grüner, David Peterhoff, Sandra Ciesek, Markus Hoffmann, Stefan Pöhlmann, Paul F. McKay, Robin J. Shattock, Roman Wölfel, Ralf Wagner, Jutta Eichler, Wolfgang Schuh, Frank Neipel, Armin Ensser, Dirk Mielenz, Matthias Tenbusch, Thomas H. Winkler, Thomas Grunwald, Klaus Überla, Hans-Martin Jäck, bioRxiv, 2021.04.16.440101; doi: https://doi.org/10.1101/2021.04.16.440101 https://doi.org/10.1101/2021.04.16.440101, https://www.biorxiv.org/content/10.1101/2021.04.16.440101v1
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: ACE2, Antibodies, Antibody, Antigen, Assay, binding affinity, Cell, Coronavirus, Coronavirus Disease COVID-19, DNA, Electroporation, Exosomes, Fluorescence, Gene, HIV, Immunization, Immunoglobulin, Liposomes, Mouse Model, Pandemic, Prophylaxis, Protein, Receptor, Research, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Spike Protein, Syndrome, Transgenic, Vaccine

Written by
Jocelyn Solis-Moreira
Jocelyn Solis-Moreira graduated with a Bachelor's in Integrative Neuroscience, where she then pursued graduate research looking at the long-term effects of adolescent binge drinking on the brain's neurochemistry in adulthood.
Source: Read Full Article