The method of choice used for preparing tissue samples can lead to biased results in the analysis of cancer patient survival. For microscopical analysis, full tissue samples provide a better picture of the immune cell activity in the tumor compared to tissue-sparing punch biopsies. A team led by the visceral surgeon Elisabeth S. Gruber and the molecular pathologist Lukas Kenner from MedUni Vienna demonstrated these findings by immunohistochemical investigation of tumor tissue of rectal cancer patients. With the second method, the density of immune cells in the tumor can be underestimated, which might result in a biased survival prognosis. The study has been published in the top journal Cancers.
In order to perform a microscopic analysis of a tissue sample, a paraffin section must be prepared. For this, the tissue sample is preserved and subsequently dehydrated and embedded in paraffin blocks. Further on, thin tissue sections of the samples are produced and applied to glass slides. Regularly, a tissue section of the whole surgical specimen of each patient is applied to one slide, so that the full extent of the tumor section is available for analysis.
For quick and efficient microscopic analysis of tumors of multiple patients, small punches of paraffin tumor tissue are compiled to one slide. This so-called Tissue Microarray (TMA) is a tissue-sparing procedure that minimizes the costs of expensive immunohistochemical analyses. Both methods allow the staining of specific protein molecules in the tumor. Digital scanning of the tissue slides allows to quantify the stained protein molecules and assign them to specific tumor compartments by the use of a special software.
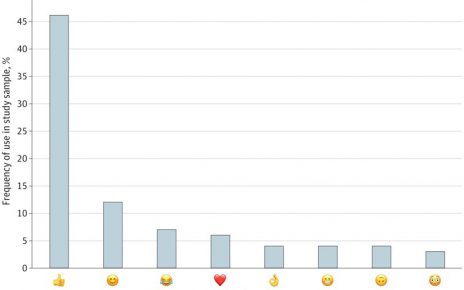
As part of this immunohistochemical study, Elisabeth S. Gruber from MedUni Vienna’s Department of Surgery and Lukas Kenner from the Department for Experimental and Laboratory Animal Pathology at MedUni Vienna, examined the amount of T cells, as important players in tumor immune surveillance, in tissue samples of 75 patients operated on for rectal cancer. One cohort of patients received radiotherapy before the surgery, the other did not. The initial study hypothesis was that radiotherapy modulates tumor immune cell infiltration. In rectal cancer, the density of T cells present in the tumor is crucial for the patient’s survival. Here, analysis was done using a special software, developed in collaboration with the Viennese company TissueGnostics, that allows analysis of a virtually established TMAs.
Source: Read Full Article