The omicron variant escapes the immune response better than other SARS-CoV-2 variants and their related coronaviruses in humans, bats and pangolins. This finding, published by a research team led by Duke-NUS Medical School and the National Center for Infectious Diseases (NCID), in the journal Nature Microbiology, suggests that omicron evolved from its ancestors to escape immunity from past infection or vaccination, especially that conferred by neutralizing antibodies, in humans during the COVID-19 pandemic.
“We present data indicating that SARS-CoV-2 variants have emerged under immune selection pressure and are evolving differently from related sarbecoviruses circulating in animals with less or no immune selection,” said senior co-author of the study Professor Wang Linfa, from Duke-NUS’ Emerging Infectious Diseases (EID) Program. Sarbecoviruses are members of the subgenus of beta coronaviruses that encompass SARS-CoV-1, which caused the SARS epidemic in 2003, SARS-CoV-2, which is responsible for the current COVID-19 pandemic, and multiple coronaviruses in bats and pangolins that have the potential to infect humans.
The omicron variant is better at escaping the immune response, but it has also helped the highly vaccinated and boosted populations to transition to living with COVID-19.
Senior co-author Professor David Lye, director, Infectious Disease Research and Training Office, NCID, explained, “Omicron’s higher transmissibility has resulted in more people acquiring hybrid immunity, which protects better against reinfection and confers mucosal immunity. Mucosal immunity refers to an immune response in the mucosa, particularly the membrane lining of the nose and throat. Many respiratory viruses first enter the body through these passages, so, boosting localized immunity in these locations can halt pathogens before they spread to the rest of the body.
“A recent study by Duke-NUS found that long-lasting SARS-CoV-2-specific T cells were found in the nasal passages of people who had breakthrough infections following vaccination. Omicron infections in vaccinated and boosted patients are also much milder with much lower rates of lung infections and need for oxygen support.”
Additionally, people who had received the Pfizer BioNTech vaccine and had been infected with SARS-CoV-2 had broader immune responses compared to those who had received the vaccine but had not been infected.
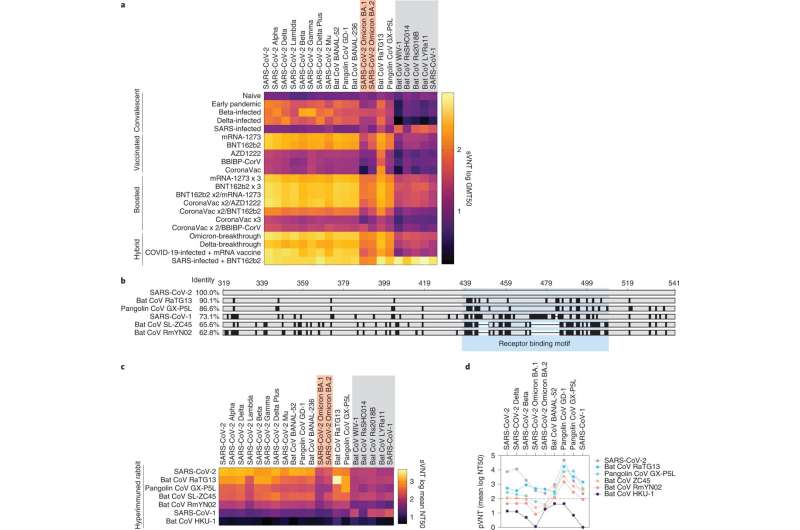
Prof. Wang and Prof. Lye were part of an international effort, including scientists in Singapore, Thailand, South Africa, Germany and the U.K., that analyzed immune responses against a variety of sarbecoviruses. They did this by investigating how well serum from people with different immune states was able to neutralize 20 different sarbecoviruses from humans, bats and pangolins, including omicron.
Variants generated in humans during the COVID-19 pandemic were able to escape neutralizing antibodies more efficiently than the sarbecoviruses that originated in animals, providing evidence that variants of concern (VOCs), especially omicron, arose under immune pressure in humans.
Source: Read Full Article



