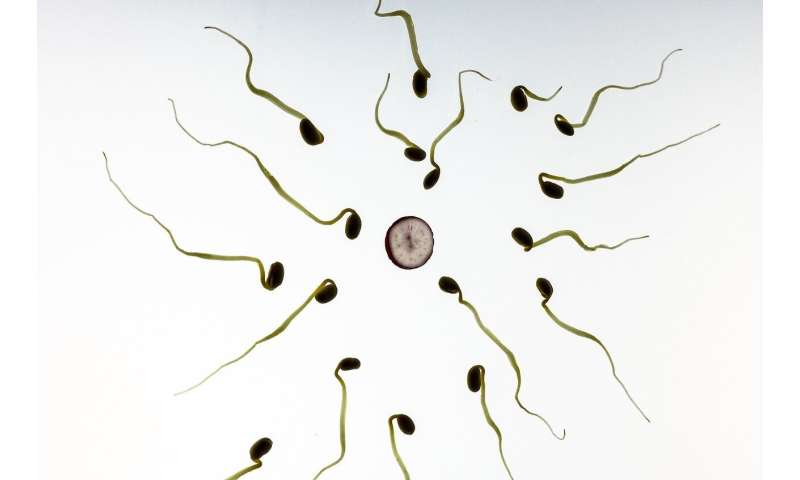
Researchers at the University of Massachusetts Amherst have identified a single-measure biomarker in sperm mitochondrial DNA that may predict male reproductive health and pregnancy success.
The discovery applies not just to couples seeking care for infertility but also for the general population. This biomarker could become a more accurate predictor of male infertility than semen parameters, on which health care organizations and clinicians have long relied.
“Clinically, the diagnosis of male infertility really hasn’t changed in decades,” says UMass Amherst environmental epigeneticist Richard Pilsner, corresponding author of the study published today, Oct. 6, in the journal Human Reproduction. “In the last 10 to 20 years, there have been major advances in the understanding of the molecular and cellular functions of sperm, but the clinical diagnosis hasn’t changed or caught up.”
In addition to Pilsner, the team of UMass researchers included lead author Allyson Rosati, who wrote the paper as part of her undergraduate honors thesis and recently completed a master’s in molecular and cellular biology; Brian Whitcomb, associate professor of epidemiology in the School of Public Health and Health Sciences. They collaborated with reproductive and perinatal epidemiologist Germaine Buck Louis, dean of the College of Health and Human Services at George Mason University, and Sunni Mumford and Enrique Schisterman at the National Institute of Child Health & Human Development.
“This project is a really nice example of interdisciplinary work and team science,” Whitcomb says. “This research required measurement of biomarkers in the laboratory combined with statistical modeling. Answering scientific questions like this one benefits from a broad range of expertise.”
Mitochondrial DNA is maternally inherited, and sperm mitochondrial DNA copy number (mtDNAcn) typically decreases eight-to-10 fold during spermatogenesis to ensure that it is low upon fertilization. In previous research by Pilsner, Whitcomb and others, increased mtDNAcn and mitochondrial DNA deletions (mtDNAdel) were associated with decreased semen quality and lower odds of fertilization in men seeking fertility treatment.
“The logical next step was to determine if the associations between sperm mitochondrial biomarkers and fertilization among couples seeking infertility treatment could be extended to couples from the general population,” Pilsner says.
The researchers accessed sperm samples from the Longitudinal Investigation of Fertility and the Environment (LIFE) study, which recruited 501 couples from Michigan and Texas from 2005 to 2009 to examine the relationships between lifestyle, including environmental chemicals, and human fertility.
They assessed sperm mtDNAcn and mtDNAdel from 384 semen samples and analyzed their association with the probability of pregnancy within one year. They found that men with higher sperm mtDNAcn had as much as 50% lower odds of cycle-specific pregnancy and 18% lower probability of pregnancy within 12 months.
“Remarkably, we saw a strong inverse association between sperm mitochondrial biomarkers and couples’ time-to-pregnancy,” Pilsner says.
Adds Whitcomb, “Mitochondrial DNA in sperm seems to reflect some underlying physiological phenomenon that affects sperm function.”
More research is needed to further examine the impact of changes in mtDNAcn and mtDNAdel, which may result from defective mitochondria or damaged mtDNA. “We need to take advantage of our understanding of the molecular toolkit that we have to develop a better predictor of male fertility, as well as fecundability,” Pilsner says.
A next step is to examine the factors mediating the changes in sperm mitochondrial DNA. They could include environmental toxins or other causes of inflammation and oxidative stress, the scientists hypothesize.
Source: Read Full Article



