The role of artificial intelligence, or machine learning, will be pivotal as the industry wrestles with a gargantuan amount of data that could improve—or muddle—health and cost priorities, according to a National Academy of Medicine Special Publication on the use of AI in health care.
Yet, the current explosion of investment and development is happening without an underpinning of consensus of responsible, transparent deployment, which potentially constrains its potential.
The new report is designed to be a comprehensive reference for organizational leaders, health care professionals, data analysts, model developers and those who are working to integrate machine learning into health care, said Vanderbilt University Medical Center’s Michael Matheny, MD, MS, MPH, Associate Professor in the Department of Biomedical Informatics, and co-editor of AI in Healthcare: The Hope, The Hype, The Promise, The Peril.
“It’s critical for the health care community to learn from both the successes, but also the challenges and recent failures in use of these tools. We set out to catalog important examples in health care AI, highlight best practices around AI development and implementation, and offer key points that need to be discussed for consensus to be achieved on how to address them as an AI community and society,” said Matheny.
Matheny underscores the applications in health care look nothing like the mass market imagery of self-driving cars that is often synonymous with machine learning or tech-driven systems.
For the immediate future in health care, AI should be thought of as a tool to support and complement the decision-making of highly trained professionals in delivering care in collaboration with patients and their goals, Matheny said.
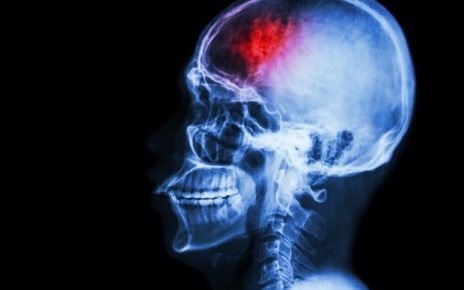
Recent advances in deep learning and related technologies have met with great success in imaging interpretations, such as radiology and retina exams, which have spurred a rush toward AI development that brought first, venture capital funding, and then industry giants. However, some of the tools have had problems with bias from the populations they were developed from, or from the choice of an inappropriate target. Data analysts and developers need to work toward increased data access and standardization as well as thoughtful development so algorithms aren’t biased against already marginalized patients.
The editors hope this report can contribute to the dialog of patient inclusivity and fairness in the use of AI tools, and the need for careful development, implementation, and surveillance of them to optimize their chance of success, Matheny said.
Matheny along with Stanford University School of Medicine’s Sonoo Thadaney Israni, MBA, and Mathematica Policy Research’s Danielle Whicher, Ph.D., MS, penned an accompanying piece for JAMA Network about the watershed moment in which the industry finds itself.
“AI has the potential to revolutionize health care. However, as we move into a future supported by technology together, we must ensure high data quality standards, that equity and inclusivity are always prioritized, that transparency is use-case-specific, that new technologies are supported by appropriate and adequate education and training, and that all technologies are appropriately regulated and supported by specific and tailored legislation,” the National Academy of Medicine wrote in a release.
Source: Read Full Article